- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer
UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH
Fibroids are non-cancerous growths that develop in or around the uterus of women. They are also known as uterine fibroids or leiomyomas. Fibroids can vary in size and may cause symptoms like heavy menstrual bleeding, pelvic pain, frequent urination, and fertility issues. These growths are usually not cancerous (benign) and are the most common noncancerous tumor in women and people assigned female at birth (AFAB). Uterine fibroids can cause a variety of symptoms like pain and heavy, irregular vaginal bleeding. Sometimes, a person has no symptoms and is unaware they have fibroids. Treatment for fibroids typically depends on your symptoms.
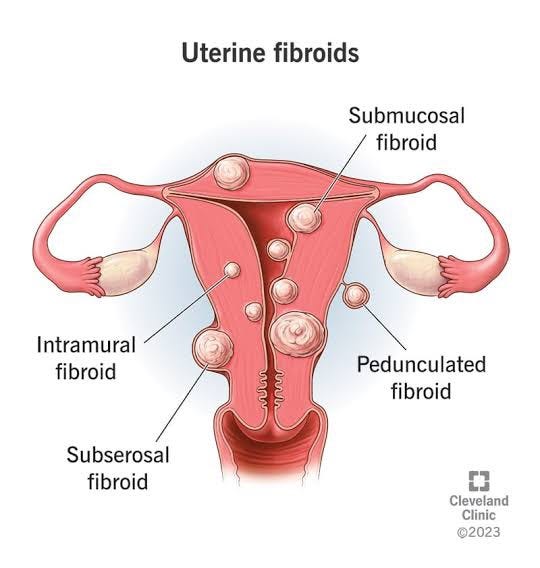
TYPES OF UTERINE FIBROIDS

There are different types of uterine fibroids depending on where they’re located and how they attach. Specific types of uterine fibroids include:
Intramural fibroids: These fibroids are embedded into the muscular wall of your uterus. They’re the most common type.
Submucosal fibroids: These fibroids grow under the inner lining of your uterus.
Subserosal fibroids: This type of fibroid grows under the lining of the outer surface of your uterus. They can become quite large and grow into your pelvis.
Pedunculated fibroids: The least common type, these fibroids attach to your uterus with a stalk or stem. They’re often described as mushroom-like because they have a stalk and then a wider top.
DELVING INTO THE CAUSES OF INFERTILITY
The exact cause of fibroids is not fully understood, but several factors are believed to contribute to their development:
-
Hormones: Estrogen and progesterone, two hormones that regulate the menstrual cycle, are thought to play a significant role in fibroid growth. Fibroids tend to grow during reproductive years when hormone levels are higher and often shrink after menopause when hormone levels decline.
-
Genetic factors: There is evidence to suggest that certain genetic changes may increase the likelihood of developing fibroids. If you have a family history of fibroids, you may be at a higher risk.
-
Hormonal imbalances: Other hormonal imbalances, such as insulin-like growth factor (IGF), may also influence fibroid growth.
-
Growth factors: Certain growth factors, like transforming growth factor-beta (TGF-beta), may be involved in the development and growth of fibroids.
-
Blood vessel abnormalities: Abnormalities in the blood vessels within the uterus could contribute to the growth of fibroids.
-
Race and ethnicity: Research has shown that women of African descent are more likely to develop fibroids compared to women of other ethnicities.
-
Lifestyle factors: Obesity and a diet high in red meat and low in fruits and vegetables have been associated with an increased risk of fibroids.
It’s important to note that while these factors may increase the risk of fibroids, the exact cause can vary from woman to woman. Additionally, most women with fibroids do not experience any symptoms or complications, and the growths often remain small and require no treatment. However, if fibroids cause bothersome symptoms or affect fertility, medical intervention may be necessary. Consulting a healthcare professional is crucial for a proper diagnosis and management plan tailored to individual needs.
SPOTTING OF SYMPTOMS: SYMPTOMS OF FIBROIDS
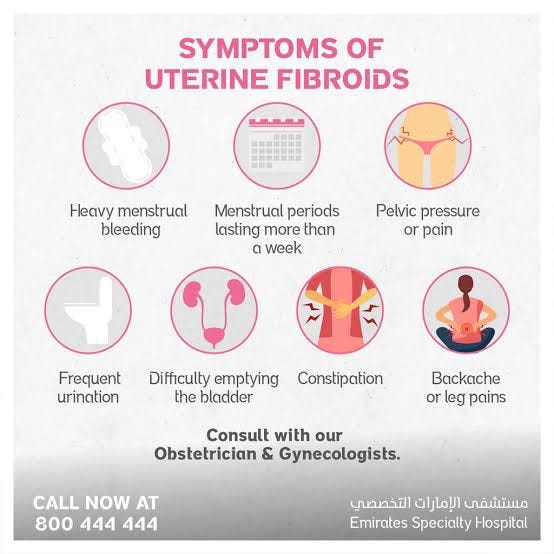
Fibroids can cause a variety of symptoms, and their severity can vary depending on the size, number, and location of the fibroids. Some common symptoms of fibroids include:
-
Heavy menstrual bleeding: Experiencing prolonged and heavy menstrual periods is a common symptom of fibroids. This can lead to anemia in some cases due to excessive blood loss.
-
Pelvic pain: Fibroids can cause pain or discomfort in the pelvic region, including lower back pain.
-
Pressure or fullness in the abdomen: Large fibroids or multiple fibroids can cause the uterus to expand, leading to a feeling of pressure or fullness in the abdominal area.
-
Frequent urination: Fibroids located near the bladder can put pressure on it, causing frequent urination or the urge to urinate frequently.
-
Difficulty emptying the bladder: In some cases, fibroids can obstruct the normal flow of urine, leading to difficulty in fully emptying the bladder.
-
Constipation: Large fibroids can press against the rectum, causing constipation or difficulty passing stool.
-
Pain during sexual intercourse: Fibroids can lead to pain or discomfort during sexual intercourse.
-
Abdominal swelling: Enlarged fibroids can cause the abdomen to swell, making it appear larger.
-
Infertility or pregnancy complications: Depending on their location, fibroids may interfere with fertility or cause complications during pregnancy, such as preterm labor or breech presentation.
QMe is a cutting-edge hospital management software designed to revolutionize healthcare facilities worldwide. With its intelligent queue-based OPD management system, patients experience reduced waiting times and optimized appointment scheduling. The software’s comprehensive patient history and electronic health records ensure seamless access to critical medical information, enabling healthcare professionals to make informed decisions and provide personalized care. QMe’s automatic workflows streamline administrative tasks and treatment plans, enhancing overall efficiency and reducing human errors. The software’s IPD management feature enables smooth inpatient care coordination, while its TPA support simplifies insurance processes. It’s important to remember that not all women with fibroids will experience symptoms. Some fibroids may be small and asymptomatic, requiring no treatment. If you suspect you have fibroids or are experiencing any of these symptoms, it’s essential to consult a healthcare professional for proper evaluation and management.
TREATMENT
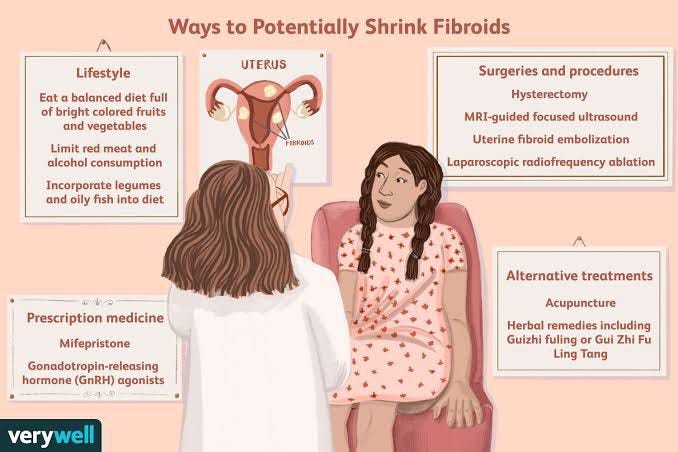
The treatment of fibroids depends on various factors, including the size and location of the fibroids, the severity of symptoms, the woman’s age, and her desire for future fertility. Treatment options for fibroids include:
-
Watchful waiting: If fibroids are small, asymptomatic, and not causing any issues, a healthcare provider may recommend regular monitoring without any immediate treatment.
-
Medications: Hormonal medications like birth control pills, progestin-releasing intrauterine devices (IUDs), or gonadotropin-releasing hormone (GnRH) agonists can help manage symptoms such as heavy bleeding and pelvic pain.
-
Non-invasive procedures: Certain minimally invasive procedures can be performed to treat fibroids, such as uterine artery embolization (UAE), where the blood supply to the fibroids is blocked, causing them to shrink.
-
Myomectomy: This surgical procedure involves the removal of fibroids while leaving the uterus intact, which may be a suitable option for women who want to preserve their fertility.
-
Hysterectomy: In cases where fibroids cause severe symptoms and other treatments are not effective, a hysterectomy, which is the surgical removal of the uterus, may be recommended. This procedure eliminates the possibility of fibroid recurrence.
-
Magnetic Resonance-guided Focused Ultrasound (MRgFUS): This non-invasive procedure uses focused ultrasound waves to destroy fibroids.
The choice of treatment depends on individual circumstances, and it’s essential to have a thorough discussion with a healthcare professional to determine the most appropriate course of action. Treatment plans should be tailored to the woman’s needs and preferences while considering the potential impact on fertility and overall health.
MYOMECTOMY & HYSTERECTOMY: A DETAILED ANALYSIS

MYOMECTOMY
Purpose: Myomectomy is performed to remove fibroids from the uterus while preserving the uterus itself. It is primarily recommended for women who desire to retain their fertility or avoid a complete removal of the uterus.
. Procedure: Myomectomy can be performed through different methods, depending on the size, number, and location of the fibroids. The three main approaches are:
.
Abdominal myomectomy: The surgeon makes an incision in the abdomen to access the uterus and remove the fibroids. This method is typically used for larger fibroids or when multiple fibroids are present.
Laparoscopic myomectomy: Minimally invasive surgery where small incisions are made in the abdomen, and a laparoscope with surgical instruments is used to remove the fibroids. This approach usually involves a shorter recovery period compared to an abdominal myomectomy.
Hysteroscopic myomectomy: A thin, lighted tube called a hysteroscope is inserted through the cervix into the uterus, allowing the surgeon to remove small fibroids that are located inside the uterine cavity.
Fertility and Pregnancy: Myomectomy may improve a woman’s chances of conceiving and carrying a pregnancy to term, especially if the fibroids were causing fertility issues. However, the success of future pregnancies after myomectomy can vary, depending on the size, number, and location of any remaining fibroids.
HYSTERECTOMY
Purpose: Hysterectomy is the surgical removal of the uterus. It is typically considered when fibroids are large, cause severe symptoms, or other treatment options have been ineffective.
TYPES OF HYSTERECTOMY
- Total Hysterectomy: The entire uterus, including the cervix, is removed.
- Subtotal or Partial Hysterectomy: The uterus is removed, but the cervix is left intact.
- Radical Hysterectomy: In cases of certain gynaecological cancers, a radical hysterectomy may be performed, which involves removing the uterus, cervix, parts of the vagina, and surrounding tissues.
Menopause and Fertility: If both ovaries are removed during a hysterectomy (oophorectomy), menopause will occur if the woman hasn’t reached menopause already. Additionally, since the uterus is removed, a woman will no longer be able to conceive or carry a pregnancy after a hysterectomy.
Both myomectomy and hysterectomy are major surgical procedures that require careful consideration. The choice between them depends on individual factors such as the woman’s age, desire for future fertility, the size and location of fibroids, and overall health. It’s essential to have a thorough discussion with a healthcare provider to fully understand the benefits, risks, and potential consequences of each procedure before making a decision. QMe offers packages support for various medical services and features automated billing to ensure transparent and hassle-free financial transactions. Embracing QMe empowers hospitals to enhance patient experiences, optimize healthcare workflows, and deliver top-notch medical services.
WHEN TO SEE A DOCTOR
See your doctor if you have:
- Pelvic pain that doesn’t go away
- Overly heavy, prolonged or painful periods
- Spotting or bleeding between periods
- Difficulty emptying your bladder
- Unexplained low red blood cell count (anemia)
PREVENTION
Unfortunately, there is no surefire way to prevent the development of fibroids as their exact cause is not fully understood. However, there are some lifestyle and health-related measures that may help reduce the risk or severity of fibroids:
-
Maintain a healthy weight: Obesity has been linked to an increased risk of fibroids, so maintaining a healthy weight through a balanced diet and regular exercise may be beneficial.
-
Eat a nutritious diet: A diet rich in fruits, vegetables, and whole grains may have a protective effect against fibroids. On the other hand, consuming a lot of red meat and processed foods may increase the risk.
-
Exercise regularly: Regular physical activity can help regulate hormone levels and promote overall health.
-
Birth control pills: Some research suggests that using oral contraceptives may reduce the risk of fibroids. However, this should be discussed with a healthcare provider based on individual needs and medical history.
-
Manage chronic conditions: Certain chronic conditions like hypertension and diabetes have been associated with an increased risk of fibroids. Properly managing these conditions may have a positive impact on fibroid risk.
-
Limit alcohol and caffeine intake: High alcohol and caffeine consumption have been linked to an increased risk of fibroids, so it’s a good idea to consume them in moderation.
-
Regular check-ups: Regular gynecological check-ups can help detect fibroids early on and monitor their growth if present.
Keep in mind that while these measures may be helpful in reducing the risk of fibroids, they cannot guarantee prevention. If you have concerns about fibroids or are experiencing symptoms, it’s essential to consult a healthcare professional for proper evaluation and guidance. Taking that on the note, QMe is a cutting-edge hospital management software designed to revolutionize healthcare facilities worldwide. With its intelligent queue-based OPD management system, patients experience reduced waiting times and optimized appointment scheduling. The software’s comprehensive patient history and electronic health records ensure seamless access to critical medical information, enabling healthcare professionals to make informed decisions and provide personalized care
RISK FACTORS
There are few known risk factors for uterine fibroids, other than being a woman of reproductive age. Factors that can have an impact on fibroid development include:
Race. Although all women of reproductive age could develop fibroids, black women are more likely to have fibroids than are women of other racial groups. In addition, black women have fibroids at younger ages, and they’re also likely to have more or larger fibroids, along with more-severe symptoms.
Heredity. If your mother or sister had fibroids, you’re at increased risk of developing them.
Other factors include
- Starting our period at an early age
- Obesity
- A vitamin D deficiency
- Having diet higher in red meat and lower in green vegetables
- Fruit and dairy
- Drinking alcohol, including beer, appear to increase your risk of developing fibroids.
HOW IS UTERINE FIBROIDS DIAGNOSED?
In many cases, a healthcare provider discovers uterine fibroids during a pelvic exam. Quite often, heavy bleeding and other related symptoms may alert your provider to consider fibroids as a part of the diagnosis. There are several tests that can be done to confirm fibroids and determine their size and location. These tests can include:
1-Ultrasonography: This noninvasive imaging test creates a picture of your internal organs with sound waves.
2-Magnetic resonance imaging (MRI): This test creates detailed images of your internal organs by using magnets and radio waves.
3-Computed tomography (CT) scan: A CT scan uses X-ray images to make a detailed image of your internal organs from several angles.
4-Hysteroscopy: During a hysteroscopy, your provider will use a device called a scope (a thin, flexible tube with a camera on the end) to look at fibroids inside your uterus. The scope is passed through your vagina and cervix and then moved into your uterus.
5-Hysterosalpingography (HSG): This is a detailed X-ray where your provider injects contrast material and then takes X-rays of your uterus.
6-Sonohysterography: In this imaging test, your provider places a small catheter in your vagina and then injects saline into your uterus. This extra fluid helps to create a clearer image of your uterus than you would see during a standard ultrasound.
7-Laparoscopy: During this test, your provider will make a small cut (incision) in your lower abdomen. A thin and flexible tube with a camera on the end will be inserted to look closely at your internal organs.
MEDICATIONS-
Over-the-counter (OTC) pain medications: These medications help manage pain and discomfort caused by fibroids. OTC medications include acetaminophen and ibuprofen.
Iron supplements: If you have anemia from excess bleeding, your provider may also suggest you take an iron supplement.
- Birth control: Birth control can also help with symptoms of fibroids – specifically, heavy bleeding during and between periods and menstrual cramps. There are a variety of birth control options you can use, including oral contraceptive pills, rings, injections and intrauterine devices (IUDs).
- Gonadotropin-releasing hormone (GnRH) agonists: These medications work by shrinking fibroids. They’re sometimes used to shrink a fibroid before surgery, making it easier to remove the fibroid. However, these medications are temporary, and if you stop taking them, the fibroids can grow back.
- Oral therapies: Elagolix is a new oral therapy to manage heavy uterine bleeding in people who haven’t experienced menopause with symptomatic uterine fibroids. It can be taken for up to 24 months. Talk to your provider about the pros and cons of this therapy. Another oral therapy, tranexamic acid, treats heavy menstrual bleeding in people with uterine fibroids.
It’s important to talk to your healthcare provider about any medication you take. Always consult your provider before starting a new medication to discuss any possible complications.
CONCLUSION
In conclusion, fibroids are non-cancerous growths that develop in or on the uterus of women during their reproductive years. They are a common condition and can vary in size and number. While the exact cause of fibroids is not fully understood, hormonal factors, genetics, and other influences may play a role in their development.
Fibroids may not cause any symptoms and can be discovered incidentally during routine check-ups or imaging tests. However, some women may experience symptoms such as heavy or prolonged menstrual bleeding, pelvic pain, frequent urination, and pressure on the bladder or bowel.
The treatment for fibroids depends on the severity of symptoms, the size and location of the fibroids, and the woman’s age and reproductive plans. Treatment options range from medication to manage symptoms, hormonal therapies to shrink fibroids, and various surgical procedures, including myomectomy and hysterectomy, to remove the fibroids or the entire uterus.
It’s essential for women with fibroids to have regular follow-ups with their healthcare providers to monitor the growth and assess any changes in symptoms. Open communication with healthcare professionals is crucial for determining the most appropriate treatment plan based on individual circumstances and preferences.
Overall, while fibroids are a common condition that can cause discomfort and impact quality of life, there are effective treatment options available to manage symptoms and improve the overall well-being of women affected by this condition.
- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer