- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer
Rashes (Eczema, Dermatitis)
Rashes (Eczema, Dermatitis)

Definition of Rashes
A rash is an obvious change in the texture or color of the skin that is frequently accompanied by redness and irritation. It can be acute or persistent and result from a number of things, including allergies, infections, or underlying disorders. To reduce discomfort, address the underlying cause, and avoid complications, proper diagnosis and care are essential. Rashes that are severe or chronic must be evaluated by a doctor.
Importance of Understanding Eczema and Dermatitis
Due to their ubiquity and effects on wellbeing, understanding eczema and dermatitis is essential. These persistent skin conditions can cause excruciating itching, discomfort, and sometimes pain. They are characterized by inflammation and irritation. Effective care not only improves the affected individuals’ quality of life but also averts consequences such skin infections. People are more able to take preventative action when they are informed about triggers, available healthcare treatments, and good skincare. Furthermore, eliminating myths and lowering stigma associated with these disorders encourages support and empathy. Accurate information is helpful in healthcare for prompt diagnosis and individualized care, underlining the significance of eczema and dermatitis awareness.
Types of Rashes

Eczema (Atopic Dermatitis)
-
Definition: Eczema and dermatitis are skin conditions characterized by inflammation, redness, and itching. Eczema, often used interchangeably with dermatitis, refers to a group of conditions that cause dry, sensitive skin. Rashes, edema, and skin thickening are characteristics. There are many different types of dermatitis, including contact dermatitis brought on by irritants or allergens. Both illnesses cause discomfort and have an impact on day-to-day life. Knowing these characteristics helps with diagnosis and treatment.
-
Causes and Triggers: Eczema and dermatitis have multifactorial origins. Genetics play a role, with inherited skin barrier dysfunction increasing susceptibility. Flare-ups may be brought on by environmental variables such allergens, irritants, and climate. Additionally, immune system responses, hormone changes, and stress can be factors. Proper skincare and trigger avoidance are essential for reducing symptoms and successfully treating these illnesses.
-
Symptoms and Clinical Presentation: Symptoms of eczema and dermatitis encompass red, inflamed skin with intense itching. Dryness, scaling, and oozing blisters may occur. In eczema, different types present distinct patterns, like nummular eczema’s coin-shaped patches. Dermatitis often manifests as localized redness or swelling upon contact with irritants or allergens. Scratching too hard might result in open sores and possible skin infections. Early identification of these symptoms enables prompt care and improves the quality of life for individuals affected.
4. Diagnosis and Differential Diagnosis: Eczema and dermatitis diagnosis requires a thorough evaluation of symptoms, medical background, and physical exam. Patch testing or skin biopsies may be used to confirm the diagnosis and pinpoint particular triggers. To identify these illnesses from other skin conditions like psoriasis or fungal infections, differential diagnosis is essential. To provide an accurate diagnosis that will allow for customized treatment regimens for efficient symptom alleviation and management, clinicians take into account the unique clinical features and test results.
Contact Dermatitis

-
Allergic Contact Dermatitis: Allergic contact dermatitis is skin inflammation triggered by allergens upon direct contact. Itching, redness, and a rash at the place of contact are symptoms. For controlling and preventing this condition, allergy avoidance, the use of hypoallergenic goods, and preventative actions are crucial.
-
Irritant Contact Dermatitis: Skin irritation brought on by immediate contact with irritants such as chemicals, detergents, or solvents is known as irritant contact dermatitis. Symptoms include redness, burning, and dryness at the contact site. For effective management and to prevent future aggravation, preventive measures like protective gloves and good skincare are essential.
-
Common Allergens and Irritants: Common allergens include nickel, fragrances, latex, and certain plants, triggering allergic reactions like contact dermatitis. Irritant contact dermatitis can be brought on by irritants such soaps, detergents, solvents, and acids. For controlling skin disorders and preventing skin responses, it’s critical to recognize and stay away from certain drugs.
4. Diagnosis and Management: Diagnosis involves clinical evaluation, medical history, and patch testing to identify specific triggers in allergic contact dermatitis. Irritant contact dermatitis is diagnosed through symptoms and exposure history. Avoiding allergens or irritating substances, utilizing emollients, topical corticosteroids, and barrier creams are all part of management. For successful symptom relief and the avoidance of recurrences, proper skincare, preventative measures, and medical assistance are crucial.
Risk Factors

Eczema and dermatitis can occur due to a number of risk factors. Genetic predisposition plays a significant role, with a family history increasing susceptibility. Environmental elements such as allergies, irritants, and weather patterns can cause symptoms to appear or worsen. People who have a history of atopic diseases like asthma or hay fever are particularly vulnerable. Certain occupations involving frequent exposure to irritants raise the risk of contact dermatitis. Moreover, stress, hormonal changes, and compromised immune function contribute. Understanding these risk factors enables the development of preventive measures, early intervention programs, and individualized management strategies for people who are prone to various skin disorders.
Pathophysiology
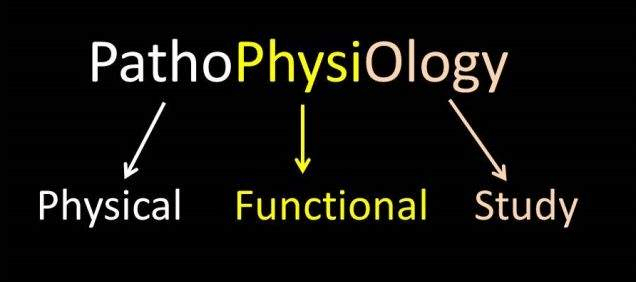
Intricate interplay between hereditary variables, immunological responses, and skin barrier failure are involved in the pathophysiology of eczema and dermatitis. Genetic predisposition contributes to impaired skin barrier function, allowing allergens and irritants to penetrate easily. Immune system problems cause increased inflammatory responses, which set off symptoms. Chronic inflammation is influenced by immune cell and cytokine dysregulation. Reduced levels of proteins like filaggrin compromise skin barrier integrity. In contact dermatitis, exposure to irritants damages the protective skin layer, inducing inflammation. Understanding these intricate pathways makes it easier to develop tailored therapeutic strategies for improving skin barrier function and controlling immunological reactions.
Clinical Assessment and Diagnosis

Examining the look, texture, and distribution of lesions on the skin in detail is necessary for the clinical assessment of eczema and dermatitis. A thorough medical history investigates the causes, course, and prior therapies. Specific allergens that cause allergic contact dermatitis can be determined through allergy testing, such as patch tests. Differential diagnosis considers similar skin conditions. Integrating clinical data and laboratory results is essential for making a correct diagnosis. Making effective treatment programs is aided by an early and precise diagnosis. In order to relieve discomfort and enhance general skin health, medical specialists are crucial in evaluating symptoms, identifying triggers, and directing patients toward the best healthcare management techniques.
Management and Treatment

Eczema and dermatitis management need a diverse strategy. General skincare includes maintaining proper hygiene, moisturizing, and avoiding irritants. Topical drugs that reduce inflammation and irritation include corticosteroids and calcineurin inhibitors. For severe cases, systemic medications such as immunosuppressants and antihistamines may be recommended. Phototherapy exposes skin to controlled UV light, reducing inflammation. Changes in lifestyle, like stress reduction and dietary modifications, can help with symptom relief. For those with these conditions, personalized healthcare management plans target the triggers, offer education, and enforce compliance, resulting in successful long-term control and an enhanced quality of life.
Coping with Eczema and Dermatitis

Managing symptoms and enhancing wellbeing are two goals of coping with eczema and dermatitis. Patients can use prescription drugs, follow good skincare practices, and steer clear of triggers. It’s crucial to adopt stress-reduction strategies and look for emotional support. Online resources and support groups offer helpful information and companionship.
The [Qme Healthcare System Software] may be very important in this procedure. It provides a thorough framework for efficient communication and collaboration between patients and healthcare professionals. From the comfort of their homes, patients can arrange virtual consultations, go over healthcare treatment plans, and get individualized advice. The app makes it easier to track the progression of symptoms, share photographs for online evaluation, and get prompt medical guidance. This streamlined method encourages patients to take an active role in their healing process, which improves symptom control and increases.
Prevention
In order to prevent eczema and dermatitis, proactive measures must be taken to reduce flare-ups. Maintain proper skincare by using mild, fragrance-free products and moisturizers. Identify and avoid known triggers like allergens or irritants, and adopt protective measures such as gloves when handling chemicals. Utilize relaxation techniques to reduce stress. For infants, breastfeeding and gentle skincare routines can reduce the risk of eczema. By giving users access to medical information, personalized recommendations, and remote monitoring, the Qme Healthcare System Software can help with prevention. This allows people to stay informed, manage potential triggers, and take prompt action to prevent exacerbations of various skin problems.
Complications
Eczema and dermatitis can lead to several complications. Chronic scratching may result in skin infections that need antibiotics. Impaired skin barrier function can lead to increased sensitivity and vulnerability to irritants. Chronic inflammation might result in lichenification, thickened and leathery skin. Psychosocial effects like anxiety, depression, and lowered self-esteem can arise due to visible symptoms. Additionally, overusing topical corticosteroids may cause other negative effects, such as skin thinning. To minimize these issues and maintain skin health and general wellbeing, proper healthcare management, preventive measures, and regular medical follow-ups are essential.
Conclusion
In conclusion, eczema and dermatitis present difficulties that interfere with comfort and mental health. For symptoms to be relieved and complications to be kept to a minimum, knowledge of triggers, prevention, and healthcare treatment is essential. With dedication to proper skincare, avoidance of triggers, and medical guidance, individuals can effectively manage these conditions. With the Qme Healthcare System Software integrated, smooth connection with medical specialists, remote monitoring, and individualized guidance are made possible. With the help of an all-encompassing strategy, patients can take control of their skin health, which improves outcomes and overall quality of life.
- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer