- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
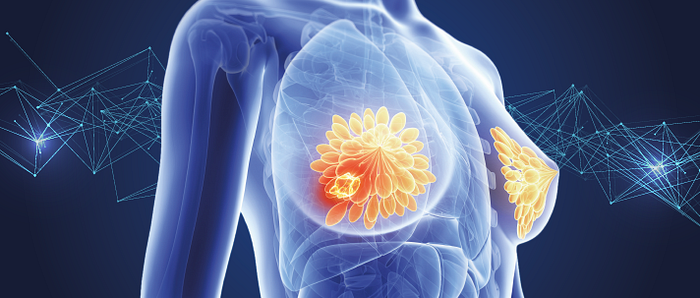
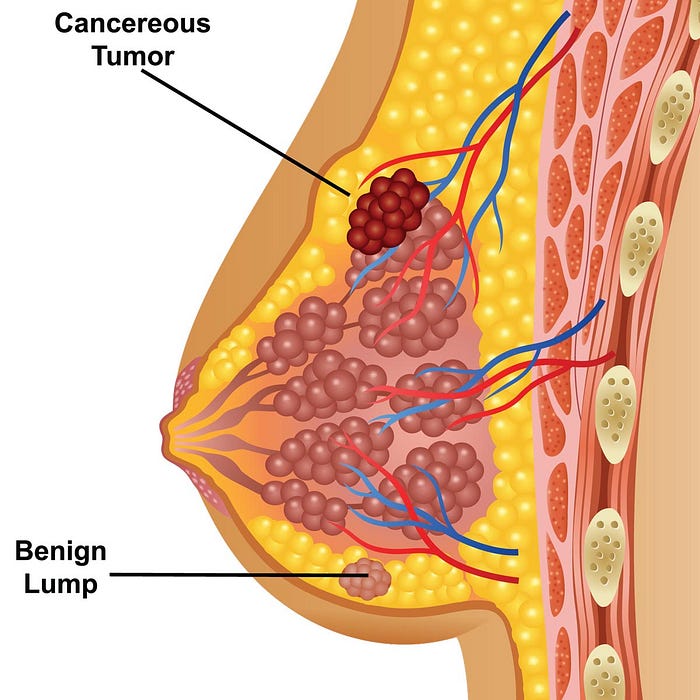
- Breast Cancer
Advances in Breast Cancer Treatment: A Comprehensive Guide
Advances in Breast Cancer Treatment: A Comprehensive Guide
Breast cancer is a serious health issue that has an enormous global impact. Given its potential for serious injury, prompt discovery and thorough healthcare treatment are absolutely essential. This manual offers a comprehensive overview of the various alternatives as it guides readers through the range of cutting-edge treatments for breast cancer. This article highlights the diverse strategy necessary for successful therapy, covering everything from targeted medications and developing tailored medicine to surgical operations like lumpectomies and mastectomy. The development of radiation therapy, chemotherapy, hormone therapy, and integrative care are examined, highlighting the interdependence between medical progress and social support. The patients’ empowerment and the teamwork of medical experts emerge as crucial forces for better results and increased quality of life as we delve into the complex landscape of breast cancer therapy.
Surgical Interventions
A. Explanation of two primary surgical options: lumpectomy and mastectomy
In a lumpectomy, the tumor is removed along with a margin of healthy tissue, leaving most of the breast intact. It is suitable for malignancies in the early stages. Mastectomy, on the other hand, involves the complete removal of the breast tissue and may be recommended for larger tumors or cases requiring preventive measures. Patient preference, tumor size, and stage guide the choice between these surgeries. Modern reconstruction methods give patients options for regaining their physical look after a mastectomy, improving their emotional and psychological well.
B. Benefits, risks, and considerations for each procedure.
The benefit of a lumpectomy is breast preservation, which produces a more natural-looking appearance. However, it requires radiation and might not suit all cases. For malignancies that are aggressive or have a genetic propensity, mastectomy gives a lower recurrence risk and is advised. However, it affects body image and requires a longer period of rehabilitation. Potential side effects like infection and scarring are possible with both surgeries. Medical considerations, patient preferences, and emotional preparation all influence decisions. Consultation with medical experts helps individuals make well-informed decisions that are in line with their needs.
C. Emerging minimally invasive techniques and their advantages.
Laparoscopic and robotic-assisted treatments are two minimally invasive surgical methods that have recently been improved upon in breast cancer surgery. Compared to conventional open operations, these procedures have smaller incisions, less discomfort, and faster recovery times. Another breakthrough is sentinel lymph node biopsy, which minimizes lymph node removal while assisting with correct staging. These methods contribute to more accurate tumor removal, better cosmetic results, and an overall improvement in quality of life throughout the recovery period in addition to improving patient comfort and satisfaction.
Radiation Therapy
A. Role of radiation therapy in breast cancer treatment post-surgery
After breast cancer surgery, radiation therapy is essential for eradicating any cancer cells that may still be present and lowering the risk of recurrence. This targeted therapy completely removes malignant tissue by efficiently destroying it. Patients who have had lumpectomies would especially benefit from it since it reduces the likelihood of cancer coming back in the area that was previously treated. Radiation therapy dramatically improves long-term results for breast cancer patients by increasing the overall effectiveness of surgical therapies.
B. Different types of radiation techniques (external beam, brachytherapy) and their applications.
External beam radiation involves directing high-energy rays from outside the body, precisely targeting the tumor site post-surgery. It’s suitable for most cases. Brachytherapy involves placing radioactive sources directly inside or near the tumor, providing a concentrated dose and limiting exposure to healthy tissue. It is frequently selected for particular situations, such as partial breast radiotherapy. Both methods seek to eliminate any remaining cancer cells while causing the least amount of harm to neighboring tissues, so enhancing healing and healthcare treatment.
C. Managing potential side effects and long-term outcomes
Benefits of radiation therapy must be weighed against potential drawbacks, including exhaustion, skin irritability, and long-term dangers including fibrosis. Close observation, skincare regimens, and lifestyle modifications assist in controlling acute consequences. Reduced side effects are a result of radiation technology advancements like intensity-modulated radiation treatment (IMRT). Regular check-ups and dialogue with medical staff enable prompt action and early detection of any issues, enabling better long-term results for breast cancer survivors.
Chemotherapy
A. Overview of chemotherapy as a systemic treatment for breast cancer
Chemotherapy is a systemic therapy that uses potent chemicals to find and kill cancer cells all over the body. When cancer has spread outside the breast, it works well. Administered orally or intravenously, chemotherapy disrupts the cancer cell’s growth cycle. Although it may have unpleasant side effects like fatigue, nausea, and hair loss, its action on cancer cells that divide quickly remains crucial. Chemotherapy frequently works in conjunction with other therapies, increasing the likelihood of effective breast cancer treatment.
B. Types of chemotherapy drugs and their mechanisms of action.
Several medication classes, including anthracyclines, taxanes, and antimetabolites, are used in chemotherapy. Anthracyclines disrupt DNA and cell division, harming the structure of cancer cells. Taxanes prevent cell division by preventing microtubule movement. Antimetabolites prevent the synthesis of DNA and RNA. Targeted treatments, such as HER2 inhibitors, target on particular proteins that support the growth of cancer. DNA damage is brought on by platinum medications. Each medicine class focuses on a separate element of cell proliferation, working together to stop cancer from spreading and promote its remission.
C. Integration of chemotherapy into different stages of breast cancer treatment.
Chemotherapy’s role in breast cancer treatment varies according to the disease stage. In neoadjuvant therapy, it’s given before surgery to shrink tumors, aiding surgical removal. Adjuvant chemotherapy follows surgery to eradicate remaining cancer cells and reduce recurrence risk. Metastatic breast cancer treatment employs chemotherapy to manage widespread disease. In order to improve the efficacy of the healthcare treatment and the results for the patients, personalized techniques establish the best timing, drug choices, and combination therapies.
D. Common side effects and strategies for managing them
Common adverse effects of chemotherapy include fatigue, reduced immunity, hair loss, nausea, and vomiting. While cold caps can reduce hair loss, antiemetic medicines can help with nausea control. Rest, a balanced diet, and mild exercise combat fatigue. Neutropenia can be managed with growth factor injections. Having open lines of communication with medical professionals supports proactive side effect treatment. Customized interventions make sure patients get the best care possible, improving their general wellbeing throughout chemotherapy.
Hormone Therapy
A. Explanation of hormone receptor-positive breast cancers.
Hormone receptor-positive (HR+) breast cancers are characterized by the presence of estrogen and/or progesterone receptors on the cancer cells. These receptors fuel the cancer’s growth in response to hormone stimulation. HR+ cancers account for a significant portion of breast cancer cases. Hormone therapy is a cornerstone of treatment, as it aims to block these receptors, depriving the cancer cells of hormonal signals and effectively slowing down or halting their growth.
B. How hormone therapy works to block estrogen and progesterone receptors
Medications that block the effects of estrogen and/or progesterone are used as part of hormone therapy for breast cancers that have hormone receptors. Selective estrogen receptor modulators (SERMs) attach to estrogen receptors, inhibiting their activation. By inhibiting the enzyme needed for estrogen synthesis, aromatase inhibitors reduce the generation of the hormone. Fulvestrant degrades estrogen receptors. Together, these methods deprive cancer cells of hormonal stimulation, slowing their growth and decreasing the likelihood that hormone-sensitive breast tumors may return.
C. Various hormone therapy drugs and their effectiveness.
Breast cancers with hormone receptors are treated with a variety of hormone treatment medications. A well-known SERM, tamoxifen, has been helpful in both pre- and postmenopausal individuals. Because they lower estrogen levels, aromatase inhibitors like letrozole and anastrozole are more suited for post-menopausal women. Fulvestrant, an estrogen receptor antagonist, is effective in advanced cases. The selection of a medication is based on the patient’s features, menopausal status, and potential adverse effects, ensuring a customized strategy for the best results.
D. Monitoring and addressing side effects of hormone therapy.
For tracking the effectiveness of hormone therapy and identifying potential side effects, routine medical exams are necessary. Joint discomfort, mood swings, and hot flushes are typical adverse effects. Exercise, dietary changes, and adequate water can all help manage these symptoms. The influence of hormone therapy on patients’ quality of life can be managed more effectively overall with timely changes made by healthcare professionals thanks to open communication between patients and medical teams.
Targeted Therapy
By focusing on particular molecular defects that fuel cancer growth, targeted therapy revolutionizes the way breast cancer is treated. Unlike traditional chemotherapy, which affects healthy cells too, targeted therapy focuses solely on cancer cells, minimizing damage to surrounding tissues. Drugs like trastuzumab block the overexpression of the HER2 protein in HER2-positive breast cancer, slowing the growth of the disease. PARP drugs take advantage of DNA repair flaws in breast tumors with BRCA mutations. These customized methods result in greater efficacy and fewer negative effects. The use of targeted therapy in conjunction with other therapies improves outcomes, ushering in a new era of customized medicine where each patient’s particular genetic profile informs treatment choices for more individualized, efficient, and patient-centered care.
Integrative and Supportive Care
Breast cancer patients receive holistic, integrative, and supportive care that takes into account all aspects of their journey — physical, emotional, and psychological. Treatment side effects are reduced and recovery is aided by individualized nutritional advice for each patient. Anxiety and depression can be treated with psychological support, such as counseling and support groups. Acupuncture, yoga, and meditation are examples of complementary therapies that promote general wellbeing. In order to maximize treatment effectiveness and quality of life, collaboration between medical experts, patients, and families promotes complete care. Integrative treatments support patients throughout their treatment course and beyond, acknowledging that wellness goes beyond the absence of disease.
Personalized Medicine and Future Directions

Through individualized treatment plans based on genetic and molecular profiles, personalized medicine revolutionizes the management of breast cancer. Unique indicators found through genomic testing help in the selection of the best medicine. Utilizing the immune system to combat cancer cells, immunotherapy has shown potential in difficult circumstances. By combining patient data, expediting diagnostics, treatment planning, and follow-ups, the QMe Hospital Management and Information System plays a crucial part. AI-driven systems that evaluate massive datasets to forecast treatment outcomes are transforming decision-making as technology develops. In the ever-changing environment of breast cancer care, this combination of customized medicine and cutting-edge healthcare systems has the potential to increase patient survival rates, reduce side effects, and improve overall wellbeing.
- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer