- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer
Gastroesophageal Reflux Disease (GERD)
Gastroesophageal Reflux Disease (GERD)
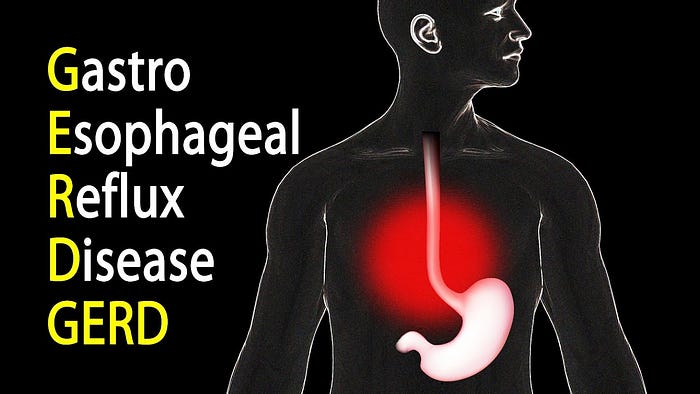
Overview
Heartburn and regurgitation are common symptoms of gastroesophageal reflux disease (GERD), a chronic digestive ailment where stomach acid commonly runs back into the esophagus. It develops as a result of the lower esophageal sphincter (LES) weakening and decreased esophageal clearance. Esophagitis and Barrett’s esophagus are just two issues that might result from GERD. Evaluation of the symptoms, endoscopy, pH monitoring, and imaging all go into the diagnosis. Treatment options include dietary adjustments, drugs such proton pump inhibitors, and, in extreme circumstances, surgery or endoscopic procedures. Improving patients’ quality of life and avoiding long-term consequences require a thorough understanding of GERD’s processes and healthcare management.
Gastrointestinal System Anatomy and Physiology

A group of interrelated organs necessary for digestion and nutrition absorption make up the gastrointestinal system. Beginning with the esophagus, it transports food to the stomach, where gastric juices aid in breakdown. The small intestine further digests and absorbs nutrients, facilitated by villi and microvilli. Bile, which is produced by the liver and stored and released by the gallbladder, is necessary for the breakdown of fats. Enzymes from the pancreas help in digestion and control blood sugar. Finally, feces are formed in the large intestine by the absorption of water and electrolytes. The coordination of hormonal signaling and muscle contractions ensures smooth operation, and the gut bacteria contributes to digesting and general health.
Pathophysiology of GERD
The frequent and inappropriate backflow of stomach contents into the esophagus is caused by a complex interplay of elements that make up the pathophysiology of gastroesophageal reflux disease (GERD). Central to this process is the malfunction of the lower esophageal sphincter (LES), a muscular ring that normally acts as a barrier preventing reflux.
Dysfunction of the LES can occur due to various reasons, including structural issues like hiatal hernias, where a portion of the stomach protrudes into the chest through the diaphragm. Obesity and pregnancy can exert pressure on the abdomen, contributing to LES relaxation. Furthermore, impaired esophageal clearance, often seen in GERD patients, allows acidic stomach contents to linger in the esophagus, exacerbating tissue damage.
Gastric acid and pepsin, digestive enzymes in the stomach, play a pivotal role in GERD. When reflux occurs, these substances irritate and injure the delicate esophageal lining, leading to inflammation (esophagitis) and potentially more severe conditions like Barrett’s esophagus, where the esophageal cells undergo precancerous changes.
Additionally, certain lifestyle factors, such as consuming large meals, lying down after eating, and consuming trigger foods (e.g., fatty or spicy foods), can exacerbate GERD symptoms. Chronic esophageal exposure to stomach acid can eventually cause erosions, strictures (narrowing of the esophagus), and chronic inflammation.
For the purpose of reducing symptoms, preventing complications, and enhancing patients’ quality of life, it is imperative to develop effective treatment strategies that promote proper esophageal clearance, restore LES function, and manage gastric acid production.
Clinical Presentation and Symptoms
Gastroesophageal Reflux Disease (GERD) manifests primarily through symptoms like heartburn and regurgitation, where stomach acid flows back into the esophagus, causing a burning sensation and sour taste. Laryngitis, a persistent cough, and chest pain are unusual symptoms. If untreated, GERD can result in side effects such esophagitis, Barrett’s esophagus, and strictures that make it difficult to swallow and cause breathing problems. For prompt diagnosis, intervention, and management of GERD, it is crucial to recognize these symptoms and any associated consequences.
Diagnosis of GERD
Patient history and symptom assessment
Obtaining a detailed patient history and conducting a thorough symptom assessment are integral to diagnosing Gastroesophageal Reflux Disease (GERD). Inquiring about frequency and severity of symptoms like heartburn, regurgitation, chest pain, and cough helps identify potential GERD cases. Understanding contributing factors can be accomplished by looking into dietary practices, lifestyle factors, and medication use. A thorough history aids in separating GERD from other illnesses and directs additional diagnostic tests for precise therapy planning.
Upper endoscopy (esophagogastroduodenoscopy)
Esophagogastroduodenoscopy (EGD), commonly known as upper endoscopy, is a diagnostic procedure that involves inserting an endoscope — a flexible tube with a camera — into the esophagus, stomach, and duodenum. The lining of the upper gastrointestinal system can be seen directly, making it easier to spot abnormalities such inflammation, erosions, ulcers, and Barrett’s esophagus. Biopsies can be taken during EGD to confirm diagnoses. This method is helpful in determining the severity of GERD-related damage and assisting with therapy choices.
pH monitoring and impedance testing
Gastroesophageal Reflux Disease (GERD) is assessed using the diagnostic procedures of pH monitoring and impedance testing. pH monitoring measures the acidity level in the esophagus over a specified period, helping to quantify reflux episodes. Impedance testing complements pH monitoring by detecting both acidic and non-acidic reflux, providing a comprehensive view of reflux patterns. Electrodes placed in the esophagus detect changes in electrical impedance caused by fluid movement. These tests assist in identifying GERD, distinguishing it from other illnesses exhibiting comparable symptoms, and directing therapy choices to effectively manage reflux.
Imaging studies (barium swallow, esophagram)
During a barium swallow, the patient ingests a contrast Gastroesophageal Reflux Disease (GERD) can be diagnosed with the help of imaging tests such an esophagram or barium swallow. Arterial (barium), which coats the esophagus and stomach, allowing X-rays to capture their structure and function. An esophagram involves taking X-ray images while the patient swallows liquid containing barium. These examinations can detect anomalies such hiatal hernias, esophageal narrowing, and modifications brought on by reflux. They support the validation of GERD diagnoses, the identification of complications, and the direction of therapeutic strategies to address underlying structural problems.
Manometry
Manometry is a diagnostic method that assesses the force and timing of esophageal muscle contractions. It helps assess the functionality of the lower esophageal sphincter (LES) and esophageal muscles, aiding in the diagnosis of Gastroesophageal Reflux Disease (GERD) and other esophageal motility disorders.
Treatment Options
Treatment for gastroesophageal reflux disease (GERD) involves dietary adjustments and weight control. Antacids, H2 receptor blockers, and proton pump inhibitors (PPIs) are examples of medications that assist manage symptoms by lowering stomach acid. Surgical interventions like fundoplication and the LINX device strengthen the lower esophageal sphincter (LES). Endoscopic treatments such as radiofrequency ablation and the Stretta procedure offer minimally invasive options to improve LES function. The selection of treatment is based on the severity of the symptoms and the preferences of the patient, with the goals of reducing discomfort, avoiding complications, and improving general quality of life.
Management of Complications
Tailored strategies are needed to manage the consequences of gastroesophageal reflux disease (GERD). Proton pump inhibitors (PPIs) and dietary adjustments can both be used to treat esophagitis. Barrett’s esophagus requires ongoing monitoring and prospective treatments include surgery and endoscopic therapy. Strictures may require dilation procedures. Optimizing GERD control and addressing related diseases are part of managing respiratory symptoms. Long-term management requires dietary changes, lifestyle adaptations, and drug compliance. Regular check-ups and monitoring aid in avoiding complications, guaranteeing the effectiveness of the treatment, and improving the patient’s general wellbeing. Each problem requires individualized approaches to ensure the best results and reduce dangers.
Patient Education and Lifestyle Strategies
Gastroesophageal Reflux Disease (GERD) patient education places a focus on lifestyle tactics to control symptoms and advance wellbeing. Encouraging smaller, frequent meals, avoiding trigger foods, maintaining a healthy weight, and elevating the head of the bed can reduce reflux. Limiting caffeine, alcohol, and smoking is advised. Meal planning, medication compliance, and post-meal activity modifications all aid in symptom control. Patients can take an active role in their care and enhance their quality of life by being taught how to recognize and react to symptom changes and the significance of long-term healthcare management and follow-ups.
Future Directions and Research
Future directions in the study of gastroesophageal reflux disease (GERD) include investigating novel therapies and gaining a better understanding of its underlying causes. Genetic and molecular research may reveal predisposition factors, enabling the development of customized treatments. Modern surgical and endoscopic methods may provide interventions that are more accurate and successful. The creation of innovative diagnostic instruments might improve monitoring and early detection. Examining how the gut microbiome affects GERD may open up new healthcare management options. Additionally, knowing how food and environmental variables affect the onset and progression of GERD can help inform preventive measures. A greater understanding of this complex illness and better outcomes are anticipated from ongoing study.
The Qme Healthcare System Software supports enhanced diagnostics, data management, and patient involvement, allowing for more individualized and well-informed GERD management decisions.
Conclusion
In conclusion, gastroesophageal reflux disease (GERD) continues to be a common and complex disorder with significant effects on patient health. We can reduce symptoms, avoid problems, and improve quality of life by thorough study of its pathogenesis, precise diagnosis, and specialized care. The significance of cutting-edge healthcare system software like Qme Healthcare System Software is becoming more and more obvious as we traverse the constantly changing environment of medical research and technology. The tools for patient involvement, improved data administration, and enhanced diagnostics offered by QMe Healthcare System Software enable healthcare providers to deliver the best treatment. Adopting such cutting-edge approaches holds the possibility of more effective, individualized, and efficient management of GERD, establishing a promising course for patient care in the future.
- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer