- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Breast Cancer
Influenza - A Silent Intruder
I. Introduction
A. Definition of Influenza (Flu)
Influenza (Flu) is a contagious diseases that causes respiratory disease caused by influenza virus(A, B, C). It spreads through respiratory droplets or contact with contaminated surfaces. A person might experience fever, cough, sore throat, muscle aches etc. The flu can lead to severe complications and is particularly dangerous for vulnerable groups. Annual flu vaccination and antiviral medications help mitigate its impact. Preventive measures, such as hand hygiene, respiratory etiquette, and staying home when sick, are essential to control its spread. Seasonal outbreaks and sporadic pandemics of influenza represent a hazard to global health, impacting people of all ages.
B. What are the various types of Influenza viruses (A, B, C). Seasonal nature and periodic pandemics
Types of Influenza Viruses:
- Influenza A:
• Most common type responsible for seasonal flu outbreaks and pandemics.
• Can infect a wide range of animals, including birds and mammals.
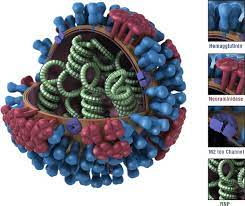
• Its various Subtypes are classified as surface proteins: Hemagglutinin (H) and Neuraminidase (N), e.g., H1N1
- Influenza B:
• Causes seasonal flu outbreaks but not pandemics.
• Mainly infects humans and can lead to similar symptoms as Influenza A but generally milder.
- Influenza C:
• Causes mild respiratory illness and is less common than Influenza A and B.
• Usually does not cause seasonal outbreaks or pandemics.
II. Causes and Transmission
A. Orthomyxoviridae family
The Orthomyxoviridae family is a group of enveloped RNA viruses that includes several important pathogens, most notably the influenza viruses. Seasonal flu outbreaks and, in certain cases, pandemics are brought on by these viruses, which pose serious risks to the public’s health.
Orthomyxoviruses have a unique structure with a lipid envelope surrounding their helical nucleocapsid core. Hemagglutinin (HA) and neuraminidase (NA), two glycoproteins found in the envelope that are essential for viral attachment, entry, and release, are present.
The viral genome of Orthomyxoviridae family members consists of multiple segments of single-stranded negative-sense RNA. This segmented genome allows for genetic reassortment when two different influenza viruses infect the same host cell. As a result, new strains with different antigenic properties can emerge, leading to the potential for novel flu virus outbreaks.
The Orthomyxoviridae family consists of three genera: Influenza A, Influenza B, and Influenza C. A wide variety of hosts are susceptible to influenza A viruses, which can infect people, birds, pigs, horses, and other animals. Based on the interaction of the proteins hemagglutinin (H) and neuraminidase (N), they are further divided into subtypes. Influenza B viruses primarily infect humans and are less prone to genetic reassortment compared to Influenza A. Compared to influenza A and B viruses, influenza C infections in humans often result in less severe respiratory symptoms.
It is crucial to comprehend the genetics, structure, and behavior of viruses of the Orthomyxoviridae family in order to create vaccines and antiviral medications that will effectively combat influenza epidemics and potential pandemics. The ever-evolving nature of influenza viruses necessitates ongoing research and surveillance to keep ahead of new strains and safeguard public health globally.
B. Transmission through respiratory droplets
Transmission of respiratory infections through respiratory droplets is a common mode of spread for many contagious diseases, including influenza, COVID-19, and other respiratory viruses. A person who is infected releases respiratory droplets into the air when they talk, sneeze, cough, or even breathe. These droplets typically contain virus particles if the person is infected.
The size of respiratory droplets is greater, and they don’t hang in the air for very long. Instead, they quickly fall to the ground or nearby surfaces within a short distance from the infected person. The exact distance droplets can travel depends on factors like the force of the cough or sneeze and environmental conditions.
The virus can infect a person’s respiratory system if these droplets come into touch with their mucous membranes (such as their mouth, nose, or eyes). This direct transmission through respiratory droplets is a significant contributor to the rapid spread of respiratory illnesses, especially in crowded places or close-contact settings.
Public health precautions including using masks, according to respiratory etiquette (covering mouth and nose when coughing or sneezing), and keeping a physical distance from other people are essential in reducing the transmission of respiratory illnesses by respiratory droplets.
II. Signs and Symptoms
A. Incubation period
The interval between being exposed to a virus or other infectious agent and developing symptoms is referred to as the incubation period. For respiratory infections like the flu or COVID-19, the incubation period is typically around 1 to 14 days, depending on the specific virus. The virus may be reproducing inside the body throughout this time, and although the infected person may not yet be sick, they may still be contagious to others.
B. Common symptoms
Common symptoms of respiratory infections like the flu or COVID-19 include fever, cough, sore throat, runny or stuffy nose, muscle or body aches, fatigue, and headache. People may occasionally also have trouble breathing or feel short of breath. It’s crucial to remember that symptoms might differ in intensity and presentation from person to person, and some infected people may experience no symptoms at all or very minor ones.
C. Variability in severity
The severity of respiratory infections like the flu or COVID-19 can vary significantly from person to person. While some people might only have minor symptoms or even remain asymptomatic, others might get seriously ill and end up in the hospital or even pass away. This heterogeneity is influenced by a number of variables, including age, underlying medical problems, and immune response. It emphasizes the significance of taking public health precautions to safeguard vulnerable groups and stop the infection’s spread.
IV. High-Risk Groups
A. Vulnerable populations (young children, elderly, pregnant women, immunocompromised)
Children, the elderly, pregnant women, those with low immune systems, and people with certain underlying medical disorders are among the vulnerable groups who are more likely to experience serious complications from respiratory infections like the flu or COVID-19.
· Young Children: Children, especially those under five years old, have developing immune systems and may have difficulty fighting off infections effectively.
· Elderly People: Older people, especially those over 65, frequently have weakened immune systems and may suffer from chronic health issues that make them more prone to serious illness.
· Pregnant Women: Pregnancy can alter the immune response, potentially increasing the risk of severe complications from certain infections.
· Immunocompromised Individuals: Those with weakened immune systems are more prone to infections and may find it difficult to properly fight off the virus, including those undergoing chemotherapy, organ transplant recipients, and those with specific medical disorders.
A crucial public health objective is to protect these vulnerable groups, and preventative interventions including immunization, hand washing, and avoiding close contact with sick people are crucial to reducing their risk of exposure to respiratory infections. Additionally, healthcare providers may consider more aggressive management and monitoring of respiratory infections in these groups to prevent severe outcomes.
B. Increased risk of complications
Children, the elderly, pregnant women, those with compromised immune systems, and people with underlying medical disorders all have a higher risk of developing serious complications from respiratory infections like the flu or COVID-19. Pneumonia, respiratory failure, the deterioration of long-term medical issues, and, in the worst situations, death, are only a few examples of these complications. To safeguard these at-risk groups’ health and safety during infectious disease outbreaks, it is essential to give them special care and take preventive measures.
V. Prevention and Control
Prevention and control of respiratory infections like the flu or COVID-19 involve a combination of public health measures and individual actions. Regular handwashing, wearing masks in crowded or high-risk settings, and practicing respiratory etiquette (covering mouth and nose when coughing or sneezing) are essential in reducing transmission. Maintaining physical distance from others, especially when social distancing measures are recommended, helps limit exposure. Public health authorities play a significant role in surveillance, early detection, contact tracing, and implementing quarantine measures to contain outbreaks. Additionally, promoting awareness and providing accurate information to the public aids in fostering responsible behaviour and adherence to preventive measures.
VI. Treatment

A. Antiviral medications
Antiviral drugs are those used to stop viruses from replicating in the body. They are used to treat viral infections like influenza and COVID-19. These medications work by targeting specific viral enzymes or proteins, preventing the virus from multiplying and spreading. When given early in the course of the infection, antiviral medications such oseltamivir for influenza and remdesivir for COVID-19 can help decrease the intensity and length of the sickness. Proper medical guidance is essential for their use.
B. Effectiveness when administered early
Early on in the course of a viral infection is when antiviral drugs are most effective. Antiviral medications can prevent viral replication and stop the spread of the virus in the body when administered quickly after the onset of symptoms. This early management may lessen the intensity of the sickness, reduce the length of the symptomatic period, and maybe avert serious complications. However, their effectiveness may diminish if initiated later in the infection, underscoring the importance of prompt medical evaluation and treatment.
The . QMe hospital management system software’s comprehensive patient history and electronic health records ensure seamless access to critical medical information, enabling healthcare professionals to make informed decisions and provide personalized care.
C. Supportive care for symptom management
Supportive care for symptom management involves providing comfort and relief to individuals with viral infections through non-specific treatments. Adequate hydration is essential to prevent dehydration, especially during illnesses that involve fever and respiratory symptoms. Rest and sufficient sleep aid the body’s recovery process. For respiratory infections, maintaining a humid environment or using a humidifier can ease breathing. The goal of symptomatic therapy is to enhance the patient’s health as the body’s immune system battles the viral infection. QMe hospital management system is a cutting-edge hospital management software designed to revolutionized healthcare facilities worldwide.
VII. Differences between Influenza Types A. Influenza A B. Influenza B C. Influenza C
Here are the key differences between them:
- Influenza A:
• Responsible for most flu outbreaks, including seasonal and pandemic flu.
• Can infect a wide range of animals, including birds, pigs, and humans.
• Classified into subtypes based on two surface proteins: Hemagglutinin (H) and Neuraminidase (N), e.g., H1N1, H3N2.
• Exhibits significant genetic variability and can undergo genetic reassortment, leading to new strains.
- Influenza B:
• Causes seasonal flu outbreaks but not pandemics.
• Primarily infects humans and is less diverse than Influenza A.
• Not classified into subtypes based on H and N proteins.
- Influenza C:
• Causes mild respiratory illness and is less common than Influenza A and B.
• Typically leads to mild symptoms and rarely causes outbreaks or epidemics.
• Not classified into subtypes and does not have the same impact as Influenza A and B.
Overall, Influenza A is the most significant in terms of its impact on human health due to its pandemic potential and ability to infect animals, while Influenza B is generally less severe and only affects humans. Influenza C is the mildest and least common among the three types.
VIII. Conclusion

In conclusion it poses a significant global health concern, leading to seasonal outbreaks and occasional pandemics. Children, the elderly, pregnant women, and people with impaired immune systems are vulnerable groups who are more likely to experience serious problems. Preventive measures like vaccination, hand hygiene, and respiratory etiquette are vital in controlling its spread. Early administration of antiviral medications can help reduce the severity of the illness. Supportive care for symptom management enhances patient comfort during the recovery process. Understanding the differences between influenza types is essential for effective management and control.
#influenzaVirus #cause #healthcareManagement #QMeHealthcare #medicalhealth #medicalhelp #treatment #prevention #healthcare
- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Breast Cancer