- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer
RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
What is Pelvic Organ Prolapse?
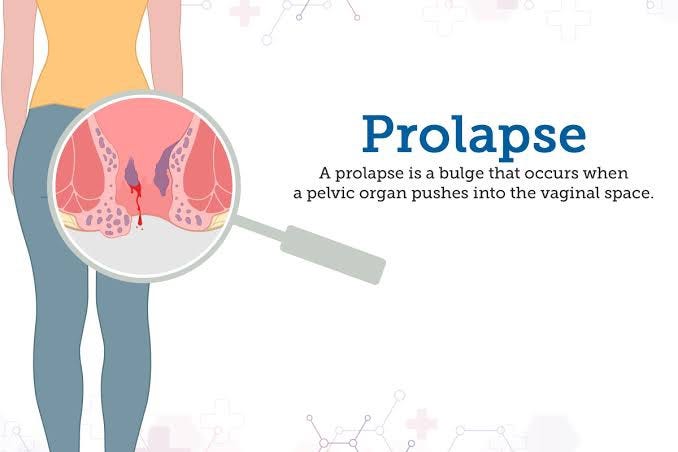
Pelvic organ prolapse (POP) is a condition in which your pelvic floor (the muscles, ligaments and tissues that support your pelvic organs) become too weak to hold your organs in place. Your pelvic floor muscles act like a powerful sling that supports organs like your vagina, uterus, bladder and rectum. If these muscles become too loose or sustain damage, the organs they support shift out of place. The pelvic organs include the vagina, cervix, uterus, bladder, urethra, and rectum.
The bladder is the most commonly involved organ in pelvic organ prolaps. With mild cases of POP, your organs may drop. In more severe cases, they may extend outside your vagina and cause a bulge.
Supporting muscles and tissue of the pelvic floor may become torn or stretched because of labor or childbirth or may weaken with age. Other risk factors for POP include: genetic predisposition, connective tissue disorder, obesity and frequent constipation.
SYMPTOMS OF PELVIC ORGAN PROLAPSE-
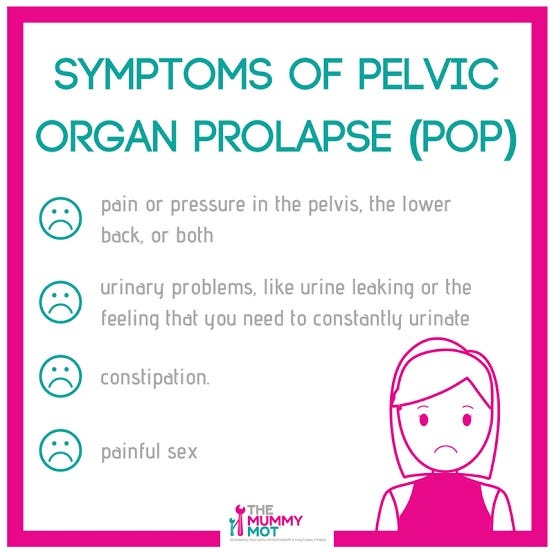
Many women have some degree of POP, although not all women have symptoms. Women who have symptoms may experience pelvic discomfort or pain, pressure and other symptoms including:
- A feeling of pressure or fullness in the pelvic area.
- A bulge or protrusion in the vaginal area, which may be felt or seen.
- Discomfort or pain in the pelvic region, lower back, or during sexual intercourse.
- Urinary problems, such as frequent urination, urgency, or difficulty emptying the bladder completely.
- Bowel issues, including constipation or difficulty having a bowel movement.
- Vaginal bleeding or spotting.
- Recurrent urinary tract infections (UTIs)
- Problems with sexual function or decreased sensation during intercourse.
It’s essential to remember that not all individuals with pelvic organ prolapse will experience all of these symptoms. Some may have mild symptoms that don’t significantly impact their daily life, while others may experience more pronounced discomfort and disruptions.
If you are experiencing any of these symptoms or suspect you might have pelvic organ prolapse, it is crucial to consult with a healthcare professional for proper diagnosis and appropriate management options. Treatment options may include pelvic floor exercises, lifestyle changes, vaginal pessaries, or, in more severe cases, surgical interventions.
CAUSES LEADING TO PELVIC ORGAN PROLAPSE-
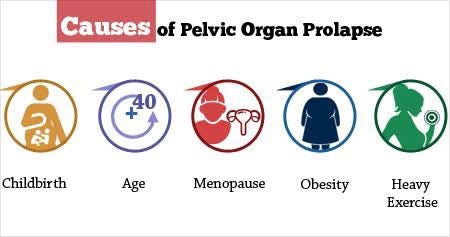
Your pelvic floor can weaken for many reasons. A weak pelvic floor increases your likelihood of a prolapse.
1- Vaginal childbirth is the most common factor associated with developing POP. Multiple vaginal deliveries, having twins or triplets, or carrying a larger than average fetus (fetal macrosomia) all increase the odds that your pelvic floor muscles will sustain injuries that may lead to POP.
2- The aging process can cause your muscles to lose strength, including your pelvic floor muscles. One factor is declining estrogen. During menopause, your body produces less estrogen. The decline can cause the connective tissues that support your pelvic floor to weaken.
3- Having a heavier body increases your risk for POP. Studies have shown that people who are clinically overweight or have obesity are more likely to develop POP than people who are in the normal weight range.
4- Long-term pressure in your abdominal cavity can overwork your pelvic floor muscles, causing them to weaken. Chronic constipation, chronic coughing and frequent heavy lifting all increase your chance of developing POP.
5- A family history of POP may increase your odds of developing POP. Research into the genetic components of POP is ongoing, but it’s possible that you inherited a weaker pelvic floor.
6-Collagen irregularities can weaken the connective tissues in your pelvic floor, increasing the likelihood you’ll develop POP. People with connective tissue disorders, like Ehlers-Danlos Syndrome, and who have more movement in their joints are at a greater risk for developing POP.
7.Hysterectomy which means surgical removal of the uterus can weaken the pelvic support structures and contribute to prolapse in some cases.
It’s essential to recognize that not all women with these risk factors will develop POP, and some women without apparent risk factors may experience pelvic organ prolapse. The severity of POP can vary, and symptoms may also differ from person to person. If any symptoms of POP are present, seeking medical evaluation and advice from a healthcare professional is crucial for accurate diagnosis and appropriate management. Treatment options for pelvic organ prolapse depend on the severity and impact of the condition on an individual’s quality of life. Taking note on that , QMe offers packages support for various medical services and features automated billing to ensure transparent and hassle-free financial transactions. Embracing QMe empowers hospitals to enhance patient experiences, optimize healthcare workflows, and deliver top-notch medical services.
What are the different types of pelvic organ prolapse?
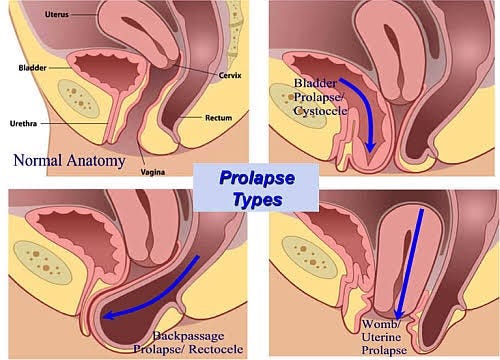
The type of prolapse you have depends on where the weaknesses are in your pelvic floor and what organs are affected.
- Anterior vaginal wall prolapse (dropped bladder): Weakened pelvic floor muscles above your vagina can cause your bladder to slip out of place and bulge onto your vagina. This type of prolapse is also called cystocele. Anterior vaginal wall prolapse is the most common type of POP.
- Urethrocele: Weakened pelvic floor muscles can cause the tube that carries pee from your bladder to outside your body (urethra) to droop. A dropped urethra often accompanies a dropped bladder.
- Posterior vaginal wall prolapse (dropped rectum): Weakened pelvic floor muscles in between your vagina and rectum can cause your rectum to bulge onto the back wall of your vagina. This type of prolapse is also called rectocele.
- Enterocele: Weakened muscles in your pelvis can cause your small intestine to bulge onto the back wall or the top of your vagina.
- Uterine prolapse (dropped uterus): A weakened pelvic floor can cause your uterus to drop down into your vaginal canal.
- Vaginal vault prolapse: Weakened pelvic floor muscles can cause the top part of your vagina (vaginal vault) to drop into your vaginal canal.
What are the Treatment Options for Pelvic Organ Prolapse?
Nonsurgical or surgical treatment is usually effective but it may not completely solve all symptoms associated with POP such as pelvic pain or pressure.
NONSURGICAL TREATMENT OPTIONS-
Examples of nonsurgical treatment options for POP include:
- Pelvic Floor Exercises: A type of exercise to strengthen the pelvic floor by contracting and relaxing the muscles that surround the opening of the urethra, vagina, and rectum. The exercises are commonly referred to as Kegels.
- Pessary: A removable device that is inserted into the vagina to support the pelvic organ(s) that have prolapsed.
SURGICAL TREATMENT OPTIONS-
Not every woman with POP will need surgery. Surgery may be recommended for women with significant discomfort or pain from POP that impairs their quality of life. If surgery is recommended, factors to consider include:
- which organs have prolapsed
- severity of prolapse
- desire for future children
- age
- sexual activity
- severity of symptomsz
Surgery to repair POP can be done through either the vagina or abdomen, using stitches (sutures) alone or with the addition of surgical mesh. Surgical options include restoring the normal position of the vagina, repairing the tissue around the vagina, permanently closing the vaginal canal with or without removing the uterus (colpocleiesis) . QMe is a cutting-edge hospital management software designed to revolutionize healthcare facilities worldwide. With its intelligent queue-based OPD management system, patients experience reduced waiting times and optimized appointment scheduling. The QMe software’s comprehensive patient history and electronic health records ensure seamless access to critical medical information, enabling healthcare professionals to make informed decisions and provide personalized care.
It is also possible that women with POP may experience problems with urine leakage (incontinence). During surgery, a procedure to prevent or decrease urine leakage (which may also use surgical mesh) may be performed.
How can I prevent pelvic organ prolapse?
Many causes of POP are out of your control. But you can put healthy habits into place to reduce your risk.
- Do pelvic floor exercises daily. Having muscle control in your pelvic floor provides stronger support for your organs.
- Maintain a healthy weight. Talk to your provider about what a healthy weight means for you.
- Prevent constipation. Chronic constipation can strain your pelvic floor muscles.
- Choosing a high-fiber diet and drinking plenty of fluids can help prevent constipation.
- Don’t smoke. Smoking can lead to chronic coughing, which can put undue pressure on your abdominal cavity and strain your pelvic floor muscles.
Also, protect your pelvic floor when you lift. Get help lifting heavy objects. When lifting alone, bend your hips and knees to squat while keeping your back as straight as possible. Don’t twist your torso while you’re lifting. Correctly positioning your body prevents injury to your low back and protects your pelvic floor, too.
FREQUENTLY ASKED QUESTIONS
Q-1-Who is affected by pelvic organ prolapse?
People of all sexes can experience POP, but you’re at greater risk if you’re a woman or person assigned female at birth (AFAB). Men and people assigned male at birth (AMAB) can experience a dropped bladder and a dropped rectum.
Q-2-What can I expect if I have pelvic organ prolapse?
Your prognosis depends on your prolapse (where it’s located, it’s severity) and your goals (to have children, to continue having penetrative sex, to have a less invasive surgery, etc.). Talk to your healthcare provider about how your prolapse shapes your treatment options. Discuss how the benefits of treatment will allow you to achieve your goals, and ask about any risks that may prevent you from achieving them, too. Grounding your expectations in honest conversations with your provider will improve your experience with POP.
CONCLUSION
In conclusion, pelvic organ prolapse is a condition where the pelvic organs descend and press against the walls of the vagina due to weakened pelvic floor muscles and ligaments. It predominantly affects women, especially those who have given birth or experienced menopause. Seeking timely medical attention and diagnosis is essential if any symptoms of pelvic organ prolapse are present. QMe offers packages support for various medical services and features automated billing to ensure transparent and hassle-free financial transactions. Embracing QMe empowers hospitals to enhance patient experiences, optimize healthcare workflows, and deliver top-notch medical services.
A healthcare professional can accurately assess the condition’s severity and determine the most appropriate treatment plan, which may include pelvic floor exercises, lifestyle changes, the use of vaginal pessaries, or, in more severe cases, surgical interventions.
Moreover, preventive measures such as maintaining a healthy lifestyle, avoiding heavy lifting, practicing pelvic floor exercises, and managing chronic conditions can help reduce the risk of pelvic organ prolapse. By understanding the symptoms and taking proactive steps, women can empower themselves to manage the condition effectively and improve their overall quality of life. Remember, every individual’s experience with pelvic organ prolapse is unique, and with the right medical care and support, women can navigate this condition with confidence and comfort.
- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer