- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer
PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
PELVIC PAIN: CAUSES SYMPTOMS AND PREVENTIONS
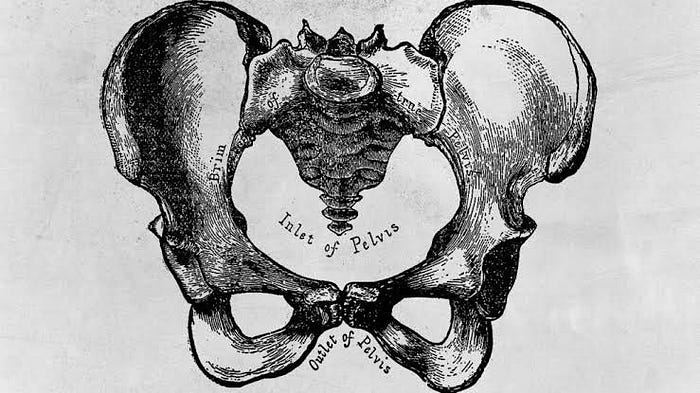
INTRODUCTION
Pelvic pain is pain in the lowest part of the stomach area and pelvis. It may be a symptom of infection or may arise from pain in the pelvic bone or in non-reproductive internal organs, such as the bladder or colon. In women, however, pelvic pain can very well be an indication that there may be a problem with one of the reproductive organs in the pelvic area (uterus, ovaries, fallopian tubes, cervix, or vagina).It affects the lowest part of the abdomen, between the belly button and groin.This article looks at causes, symptoms and treatment of Pelvic pain.
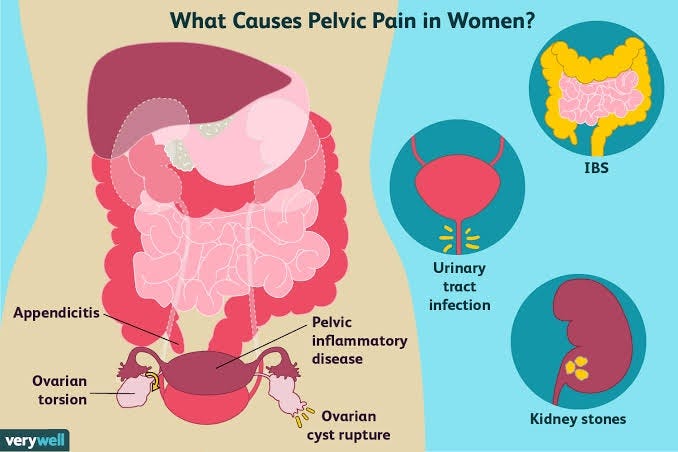
WHAT COULD BE CAUSING PAIN IN PELVIS AS A WOMEN?
MENSTRUAL PAIN AND CRAMPS-
Menstrual cramping is a common cause of pelvic pain.It typically occurs immediately before a person starts their period, as the uterus contracts and sheds its lining. The pain may feel similar to a muscle spasm or a jabbing pain.
OVULATION -
If an individual feels a painful sensation on one side of their pelvis in the middle of their menstrual cycle, they may be experiencing “mittelschmerz”. Doctors use this German word to describe painful ovulation.
When a person ovulates, the ovaries release an egg and some other fluid. The egg will then travel down the fallopian tube and into the uterus. The fluid released by the ovary can also enter the abdominal cavity and pelvis, which can cause irritation.
The discomfort may last for minutes or hours, and it may switch sides of the body, depending on which ovary released the egg. The pain is temporary and requires no specific treatment.
CYSTITIS AND URINARY TRACT INFECTION
Cystitis refers to inflammation in the bladder due to a bacterial infection. This happens because vaginal, rectal, or skin bacteria can enter the urethra, a tube that drains urine from the bladder, and travel to the bladder.
A urinary tract infection (UTI) can occur anywhere in the urinary system, while cystitis occurs only in the bladder.
PELVIC INFLAMMATORY DISEASE
Pelvic inflammatory disease (PID) is an infection in the womb that can damage the surrounding tissue. PID can arise if bacteria from the vagina or cervix enter the womb (uterus) and take hold.
PID is usually a complication of an STI, such as gonorrhea or chlamydia. Females may experience other symptoms along with pelvic pain, including abnormal vaginal discharge and bleeding.
Treatment typically involves taking antibiotics to treat the bacterial infection. However, they cannot treat scarring, so early treatment is crucial. Scarring typically occurs within the pelvic organs due to recurrent or untreated infections causing PID.
ENDOMETRIOSIS
Endometriosis occurs when tissue similar to the endometrium, or tissue that lines the inside of the uterus, grows outside of the womb. This study finds that race and ethnicity appear to play a role in the prevalence of endometriosis. However, there is limited literature examining the influence of race and ethnicity on the symptoms of endometriosis or access to healthcare and response.
Endometriosis can cause chronic, prolonged pelvic pain in some females. When a person’s period begins, the tissue outside of the uterus responds to hormonal changes, which may cause bleeding and inflammation in the pelvis.
Some people may experience mild to severe pain. Endometriosis may make it difficult for some women to become pregnant.
IRRITABLE BOWEL SYNDROME (IBS)
Irritable bowel syndrome (IBS) is a gut disorder that causes pain and symptoms, including constipation, diarrhea, and bloating.
IBS symptoms tend to flare up and go away over time, especially after a bowel movement. There is no cure for IBS, so treatment focuses on managing symptoms through changes in diet, stress levels, and medications.
APPENDICITIS
Appendicitis is inflammation in the appendix, which is a small organ in the lower-right abdomen. An infection causes this condition, and, although common, it can be severe.
URINARY STONES
Stones in the urinary tract consist of salts and minerals, such as calcium, that the body has trouble getting rid of in the urine.
These minerals can build up and form crystals in the bladder or kidneys that often cause pain in the pelvis or lower back. Stones may also cause the urine to change color, often turning it pink or reddish with blood. Sometimes, a doctor may recommend medications to break up stones or surgery to remove them.
OVARIAN CYSTS
Ovarian cysts occur when the ovaries fail to release an egg. The follicle holding the egg may not open entirely or become clogged with fluid.
When this happens, a growth called a cyst forms in the area, which may cause bloating, pressure, or pelvic pain on the side of the body with the cyst. Doctors can identify ovarian cysts using ultrasound, and they may recommend treatments that range from watchful waiting to surgery.
TUMOUR
In rare cases, a malignant growth in the reproductive system, urinary tract, or gastrointestinal system may be the reason for pain in the pelvis. The tumour may also cause other symptoms, depending on where it appears.
Doctors will perform a thorough evaluation, often using blood and imaging tests, to identify a tumour. Once they have diagnosed the issue, they will recommend possible treatments.
CAUSES OF PAIN IN MEN-

Some conditions that cause pelvic pain may be due to conditions specific to the male reproductive system such as-
BACTERIAL PROSTATITIS
Prostatitis refers to inflammation and swelling of the prostate gland. Bacterial prostatitis is an infection of the gland caused by bacteria. Along with pelvic pain, symptoms can include:
- a frequent or urgent need to urinate
- painful urination
- inability to pass urine
- fever
- chills
CHRONIC PELVIC PAIN
If you have long-term pelvic pain with no infection or other obvious cause, you will likely receive a diagnosis of chronic pelvic pain syndrome. To qualify for this diagnosis, you need to have had pelvic pain for at least 3 months. People with this condition have pain in the penis, testicles, the area between the testicles and rectum (perineum), and lower belly.
Other symptoms include:
- pain during urination and ejaculation
- a weak urine stream
- an increased need to urinate
URETHRAL STRICTURE
The urethra is the tube that urine passes through from the bladder out of the body. Urethral stricture refers to a narrowing or blockage in the urethra caused by swelling, injury, or infection. The blockage slows the flow of urine out of the penis. Symptoms of urethral stricture include pain in the abdomen and:
- a slow urine stream
- pain while urinating
- blood in the urine or semen
- leaking of urine
Temporary and mild pelvic pain is probably nothing to worry about. If the pain is severe or continues for more than several days, make an appointment with a doctor. QMe offers packages support for various medical services and features automated billing to ensure transparent and hassle-free financial transactions. Embracing QMe empowers hospitals to enhance patient experiences, optimize healthcare workflows, and deliver top-notch medical services.
TREATMENT OF PELVIC PAIN
Treatment of pelvic pain involves a comprehensive approach, addressing the underlying cause and providing symptom relief. Here’s a more detailed overview of potential treatments:
Medical Evaluation:
The first step is to visit a healthcare professional for a thorough medical evaluation. They will take a detailed medical history, perform a physical examination, and may order diagnostic tests, such as imaging or lab work, to identify the cause of the pelvic
Medications:
Depending on the diagnosis, different medications may be prescribed to manage pelvic pain. These can include:
Pain relievers: Over-the-counter pain medications (e.g., acetaminophen, ibuprofen) or prescription-strength drugs to alleviate pain and inflammation.
Hormonal therapy: For conditions like endometriosis or certain menstrual disorders, hormonal medications may be used to regulate hormone levels and reduce pain.
Antibiotics: If pelvic pain is caused by an infection, antibiotics may be prescribed to treat the underlying infection.
Physical Therapy:
Pelvic floor physical therapy can be beneficial for certain types of pelvic pain. Specially trained physical therapists can help improve muscle strength, flexibility, and function in the pelvic region, potentially reducing pain and discomfort.
Lifestyle Changes:
Adopting certain lifestyle modifications can also contribute to pain management. For instance:
Dietary changes: Avoiding trigger foods that may exacerbate pelvic pain, especially in conditions like irritable bowel syndrome (IBS).
Stress management: Techniques like yoga, meditation, or deep breathing exercises may help alleviate pelvic pain related to tension and stress.
Surgical Interventions:
In some cases, surgical procedures may be necessary to address the underlying cause of pelvic pain. Conditions such as endometriosis, fibroids, ovarian cysts, or certain reproductive organ issues might require surgical intervention.
Counseling or Psychotherapy: For cases where pelvic pain is linked to psychological factors like anxiety or depression, counseling or psychotherapy can be beneficial in managing the pain.
Complementary and Alternative Therapies:
Some people find relief from pelvic pain through complementary treatments, such as acupuncture, chiropractic care, or herbal supplements. However, it’s crucial to consult with a healthcare provider before trying these methods.
It’s important to remember that pelvic pain can be complex, and its management may require a multidisciplinary approach involving various healthcare specialists.
Always consult a qualified healthcare professional to receive an accurate diagnosis and personalised treatment plan for your specific situation. They can help determine the most appropriate course of action based on your medical history, symptoms, and test results.
Additionally, QMe offers packages support for various medical services and features automated billing to ensure transparent and hassle-free financial transactions. Embracing QMe empowers hospitals to enhance patient experiences, optimize healthcare workflows, and deliver top-notch medical services.
CAN PELVIC PAIN BE PREVENTED?
Pelvic pain can’t always be prevented. However, incorporating these recommendations into your daily life can help reduce your risk:
- Don’t overuse-Limit activities that require you to stand or walk for long periods of time.
- Eat more fiber- This is particularly helpful if your pelvic pain is due to diverticulitis.
- Exercise regularly-Staying physically active helps keep your joints and muscles in good condition.Stretch your muscles- Warm up before exercising to help reduce the risk of pelvic pain.
Visit your healthcare provider regularly. Routine examinations can help your medical team detect issues early on before they worsen.QMe is a cutting-edge hospital management software designed to revolutionize healthcare facilities worldwide. With its intelligent queue-based OPD management system, patients experience reduced waiting times and optimized appointment scheduling. The software’s comprehensive patient history and electronic health records ensure seamless access to critical medical information, enabling healthcare professionals to make informed decisions and provide personalized care. QMe’s automatic workflows streamline administrative tasks and treatment plans, enhancing overall efficiency and reducing human errors.
- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer