- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer
GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
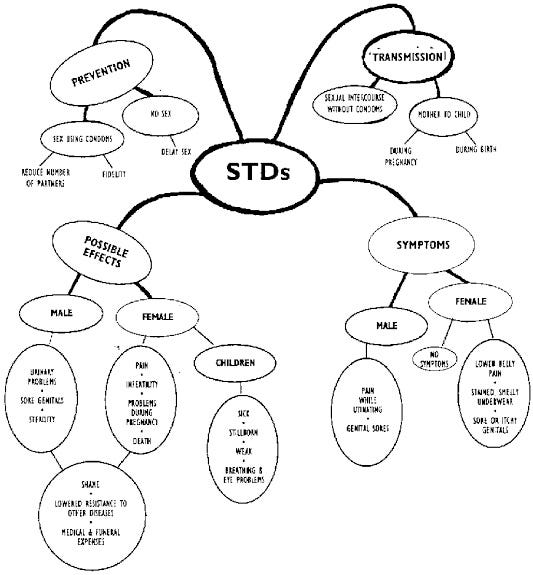
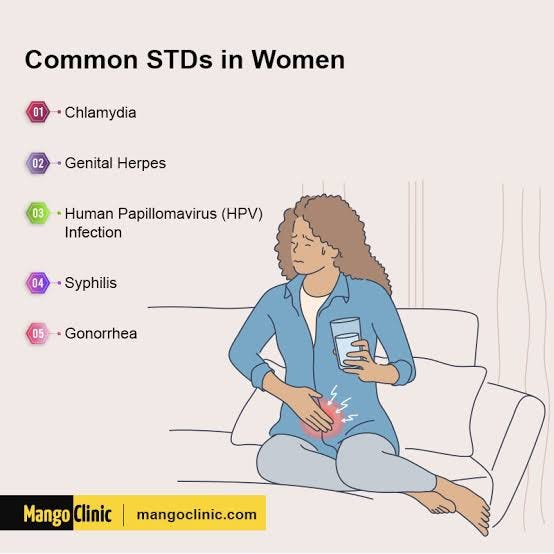
STI simply stands for “Sexually Transmitted Infection”. It is an infection that is transmitted from one person to another through sexual contact. These infections can be caused by various microorganisms, including bacteria, viruses, parasites, and fungi, and they can affect the genital, anal, and oral areas. STIs can be spread through vaginal, anal, or oral sex with an infected partner. Some of the most common STIs include chlamydia, gonorrhoea, syphilis, human papillomavirus (HPV), herpes, trichomoniasis, and human immunodeficiency virus (HIV).
Many STIs can be asymptomatic, meaning infected individuals may not show any noticeable symptoms. However, even in the absence of symptoms, STIs can still be transmitted to sexual partners. Some STIs can cause genital sores, abnormal discharge, pain or discomfort during urination, and other symptoms. This article reflects the causes, symptoms and preventions of STI and try to promote a healthier lifestyle.
CAUSES LEADING TO SEXUAL TRANSMITTED INFECTIONS

Sexually Transmitted Infections (STIs) are caused by various microorganisms that can be transmitted from one person to another through sexual contact. The main modes of transmission include vaginal, anal, and oral sex. Here are the common types of microorganisms that cause STIs:
- Bacteria: Bacterial STIs are caused by different types of bacteria. Examples include:
. a. Chlamydia trachomatis: Causes chlamydia, one of the most common bacterial. STIs.
. b. Neisseria gonorrhoeae: Causes gonorrhea, another common bacterial STI.
- Viruses: Viral STIs are caused by various viruses. Examples include:
. a. Human Papillomavirus (HPV): Causes genital warts and can lead to certain types of cancer.
. b. Herpes Simplex Virus (HSV): HSV-1 and HSV-2 can cause genital herpes, leading to painful sores or blisters.
. c. Human Immunodeficiency Virus (HIV): Causes HIV infection, which leads to acquired immunodeficiency syndrome (AIDS).
- Parasites: Parasitic STIs are caused by certain parasites. An example is:
. a. Trichomonas vaginalis: Causes trichomoniasis, a common parasitic STI.
- Fungi: Fungal STIs are caused by certain types of fungi. An example is:
. a. Candida albicans: Can cause yeast infections, including genital candidiasis.
The transmission of these microorganisms occurs through contact with infected bodily fluids, such as vaginal secretions, semen, blood, or oral fluids. The risk of transmission is higher if there are open sores, wounds, or mucous membrane exposure during sexual contact. QMe is a cutting-edge hospital management software designed to revolutionize healthcare facilities worldwide. With its intelligent queue-based OPD management system, patients experience reduced waiting times and optimized appointment scheduling. The software’s comprehensive patient history and electronic health records ensure seamless access to critical medical information, enabling healthcare professionals to make informed decisions and provide personalized care. QMe’s automatic workflows streamline administrative tasks and treatment plans, enhancing overall efficiency and reducing human errors. The software’s IPD management feature enables smooth inpatient care coordination, while its TPA support simplifies insurance processes.
SPOTTING THE SIGNS OF STI

Symptoms of Sexually Transmitted Infections (STIs) can vary depending on the type of infection and may range from mild to severe. Some STIs can be asymptomatic, meaning infected individuals show no noticeable symptoms. However, even in the absence of symptoms, STIs can still be transmitted to sexual partners. Here are some common symptoms of STIs:
-
Abnormal Genital Discharge: Unusual discharge from the penis, vagina, or anus may indicate an STI. The discharge may be yellow, green, or frothy in appearance and may have a strong odor.
-
Pain or Burning During Urination: Discomfort or pain while urinating can be a sign of certain STIs, such as chlamydia, gonorrhea, or trichomoniasis.
-
Genital Sores or Ulcers: Some STIs, such as herpes or syphilis, can cause painful sores or ulcers on or around the genitals or mouth.
-
Genital Itching or Irritation: Persistent itching or irritation in the genital area may indicate an STI, such as trichomoniasis or pubic lice (crabs).
-
Pain During Sexual Intercourse: Pain or discomfort during intercourse, known as dyspareunia, can be a symptom of certain STIs, such as chlamydia or gonorrhea.
-
Lower Abdominal or Pelvic Pain: Some STIs, like chlamydia or gonorrhea, can lead to pelvic inflammatory disease (PID) and cause pelvic pain.
-
Swollen Lymph Nodes: Enlarged or tender lymph nodes in the groin area can be a sign of an STI.
-
Rash or Redness: Certain STIs, such as syphilis or human papillomavirus (HPV), can cause skin rashes or redness.
-
Fever and Fatigue: Systemic symptoms like fever, fatigue, or body aches may occur in some STI infections.
It’s important to note that not all STIs cause noticeable symptoms, especially in the early stages of infection. Regular STI testing is crucial, especially for sexually active individuals or those with multiple sexual partners, to detect infections early and prevent complications.
If you experience any concerning symptoms or suspect you have been exposed to an STI, seek medical attention promptly for proper diagnosis and appropriate treatment. Early detection and treatment of STIs can help prevent the spread of infection and promote overall sexual health.
Additionally, QMe offers packages support for various medical services and features automated billing to ensure transparent and hassle-free financial transactions. Embracing QMe empowers hospitals to enhance patient experiences, optimize healthcare workflows, and deliver top-notch medical services.
PREVENTATIVE MEASURES
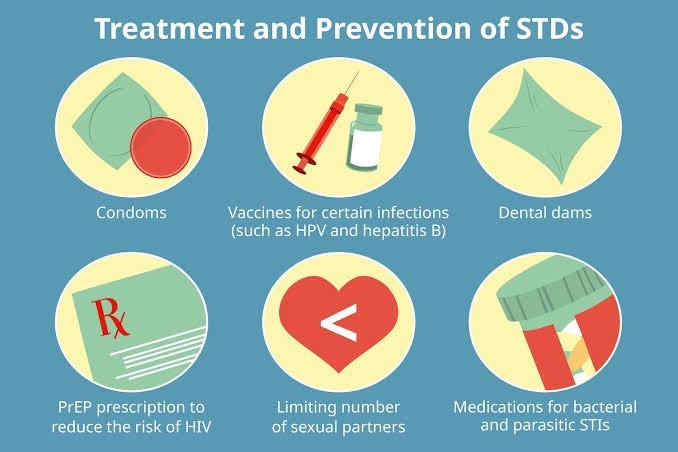
Preventing Sexually Transmitted Infections (STIs) involves taking proactive measures to reduce the risk of acquiring or transmitting these infections. Here are some key preventive measures:
-
Abstain from Risky Sexual Behavior: Abstaining from sexual activity or delaying sexual debut can reduce the risk of STIs. The only sure way to avoid STIs completely is to abstain from sexual contact.
-
Practice Safe Sex: Consistently and correctly use condoms during sexual intercourse, including vaginal, anal, and oral sex. Condoms act as a barrier, preventing the exchange of bodily fluids that can transmit STIs.
-
Limit Sexual Partners: Reducing the number of sexual partners can lower the risk of exposure to STIs. Having fewer sexual partners reduces the likelihood of encountering someone with an infection.
-
Get Regular STI Testing: If sexually active or at risk, get tested regularly for STIs, even in the absence of symptoms. Early detection allows for timely treatment and prevents further transmission.
-
Vaccination: Vaccines are available for certain STIs, such as the human papillomavirus (HPV) vaccine. Getting vaccinated can prevent infections and reduce the risk of associated complications.
-
Partner Notification and Testing: If diagnosed with an STI, notify your sexual partners, so they can get tested and treated as well. This helps prevent reinfection and further transmission.
-
Avoid Sharing Needles: If you use drugs, never share needles or syringes, as it can transmit blood-borne infections like HIV and hepatitis B and C.
-
Maintain Open Communication: Talk openly with sexual partners about STIs, testing, and safe sex practices. Honest communication can lead to better decision-making and reduced risk.
-
Know Your Partner’s Sexual History: Knowing your partner’s sexual history can help assess potential risk factors and make informed decisions about protection.
-
Practice Good Hygiene: Keeping the genital area clean and practicing good hygiene can help prevent certain infections, but it is not a substitute for safe sex practices.
It’s important to remember that no preventive measure is foolproof, and the best way to reduce the risk of STIs is to combine multiple prevention strategies. Regular STI testing and open communication with healthcare providers and sexual partners are essential for maintaining sexual health and well-being. If you suspect you have an STI or have concerns about sexual health, seek medical attention for proper diagnosis and appropriate management. Additionally, QMe offers packages support for various medical services and features automated billing to ensure transparent and hassle-free financial transactions. Embracing QMe empowers hospitals to enhance patient experiences, optimize healthcare workflows, and deliver top-notch medical services.
TREATMENT FOR THE TROUBLE
The treatment of Sexually Transmitted Infections (STIs) often involves medication to eliminate the infection and manage symptoms. The specific medication prescribed will depend on the type of STI and its severity. Here are some common medications used to treat specific STIs:
-
Chlamydia: Chlamydia is typically treated with antibiotics, such as azithromycin or doxycycline. These antibiotics help clear the bacterial infection.
-
Gonorrhea: Gonorrhea is also treated with antibiotics, most commonly with a single injection of ceftriaxone followed by an oral dose of azithromycin or doxycycline.
-
Syphilis: Syphilis is treated with antibiotics, usually penicillin or other antibiotics depending on the stage of the infection.
-
Human Papillomavirus (HPV): There is no specific medication to cure HPV, but treatments focus on managing symptoms such as genital warts. Topical treatments like podofilox or imiquimod may be used.
-
Herpes: Herpes is managed with antiviral medications like acyclovir, valacyclovir, or famciclovir. These medications help reduce the severity and duration of outbreaks and may be used for suppressive therapy.
-
Trichomoniasis: Trichomoniasis is treated with oral antibiotics, such as metronidazole or tinidazole, to eliminate the parasite causing the infection.
-
Human Immunodeficiency Virus (HIV): HIV is managed with antiretroviral therapy (ART), which is a combination of different antiretroviral medications. ART helps control the virus and improve the immune system function, but it does not cure HIV.
It’s essential to take prescribed medications as directed by a healthcare professional and to complete the full course of treatment, even if symptoms improve. Stopping medications prematurely can lead to incomplete eradication of the infection and may contribute to drug resistance.
Along with medication, lifestyle changes, such as practicing safe sex, using condoms consistently and correctly, limiting sexual partners, and getting regularly tested for STIs, are crucial for preventing further transmission of STIs and maintaining sexual health. Taking note on that, QMe is a cutting-edge hospital management software designed to revolutionize healthcare facilities worldwide. With its intelligent queue-based OPD management system, patients experience reduced waiting times and optimized appointment scheduling. The software’s comprehensive patient history and electronic health records ensure seamless access to critical medical information, enabling healthcare professionals to make informed decisions and provide personalized care. QMe’s automatic workflows streamline administrative tasks and treatment plans, enhancing overall efficiency and reducing human errors. The software’s IPD management feature enables smooth inpatient care coordination, while its TPA support simplifies insurance processes
Frequently Asked Questions about Sexually Transmitted Infections (STIs):

Q: Can STIs be asymptomatic?
. A: Yes, many STIs can be asymptomatic, meaning infected individuals show no noticeable symptoms. Asymptomatic individuals can still transmit STIs to sexual partners.
Q: How are STIs diagnosed?
. A: STIs are diagnosed through medical history, physical examination, and laboratory tests. Testing may involve urine samples, blood tests, swabs from the genital or oral areas, or tissue samples.
Q: Can STIs be cured?
. A: Some STIs, such as bacterial infections like chlamydia and gonorrhea, can be cured with appropriate antibiotic treatment. However, viral infections like HIV and herpes have no cure, but symptoms can be managed with antiviral medications.
Q: Is HIV the same as AIDS?
. A: No, HIV (Human Immunodeficiency Virus) is the virus that causes HIV infection. AIDS (Acquired Immunodeficiency Syndrome) is the late stage of HIV infection, characterized by severe immune system damage and opportunistic infections.
Q: Can I get an STI from oral sex?
. A: Yes, STIs can be transmitted through oral sex, including infections like chlamydia, gonorrhea, syphilis, herpes, and HPV.
Q: Should I notify my sexual partners if I have an STI?
. A: Yes, it’s crucial to notify your sexual partners if you have been diagnosed with an STI. Partner notification helps prevent further transmission and ensures that partners can seek testing and treatment.
Q: Can I get an STI from a toilet seat?
. A: No, STIs cannot be transmitted through casual contact with toilet seats or other surfaces. STIs are primarily transmitted through sexual contact or sharing contaminated needles.
Q: Do I need to get tested for STIs if I have no symptoms?
. A: Yes, regular STI testing is essential, even if you have no symptoms, especially if you are sexually active or have multiple sexual partners. Many STIs can be asymptomatic, and early detection is crucial for timely treatment and prevention of complications.
Remember, it’s essential to consult a healthcare professional for accurate information, testing, and appropriate treatment for any concerns or questions regarding STIs and sexual health.
CONCLUSION
In conclusion, Sexually Transmitted Infections (STIs) are infections caused by various microorganisms that can be transmitted from one person to another through sexual contact. STIs can have mild to severe symptoms or even be asymptomatic, making regular testing crucial for early detection and treatment. Preventing STIs involves practicing safe sex, using condoms consistently and correctly, limiting sexual partners, and getting vaccinated when available.
Proper treatment for STIs typically involves medication, but the specific approach depends on the type of infection. Antibiotics are commonly used for bacterial STIs like chlamydia and gonorrhea, while antiviral medications manage viral infections like herpes and HIV. Regular STI testing and open communication with healthcare providers and sexual partners are essential for maintaining sexual health.
Remember, early detection and appropriate treatment of STIs are crucial to prevent complications and promote overall sexual health. If you suspect you have an STI or have concerns about sexual health, seek medical attention for proper diagnosis and treatment. Engaging in safe sexual practices, staying informed, and maintaining open communication with sexual partners are fundamental aspects of promoting sexual health and reducing the spread of STIs.
- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer