- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer
Pancreatic Cancer
Unraveling Pancreatic Cancer: Understanding, Challenges, and Advances
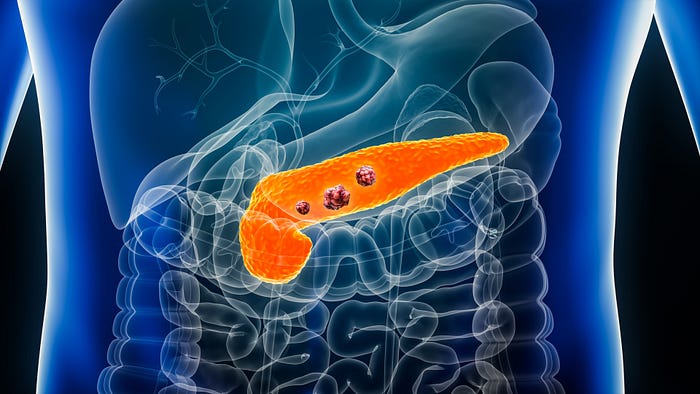
Pancreatic Cancer
Pancreatic cancer, a devastating healthcare challenge, arises from abnormal cell growth in the pancreas — a vital organ regulating digestion and blood sugar levels. With a low early detection rate, it often advances unnoticed until later stages, complicating treatment options. Risk factors, including smoking, obesity, and genetic predisposition, underscore the need for proactive healthcare strategies. As a notorious culprit behind high mortality rates, pancreatic cancer necessitates heightened public awareness, improved screening methods, and enhanced research efforts to develop effective treatments. This introduction sheds light on the critical intersection of healthcare, early diagnosis, and innovative solutions in addressing this formidable disease.
Epidemiology and Risk Factors
Pancreatic cancer exhibits a concerning epidemiological pattern, with a higher incidence in older individuals and specific demographics. Prominent risk factors, such as smoking, obesity, and family history, significantly contribute to its development. Genetic mutations like BRCA1 and BRCA2 also play a role, along with conditions like chronic pancreatitis and diabetes. This interplay between demographic and genetic elements underscores the complexity of pancreatic cancer’s origin. An understanding of these epidemiological factors provides crucial insights into targeted prevention strategies and early detection efforts, offering potential pathways to mitigate the impact of this aggressive disease on public health.
Pathophysiology
Pancreatic cancer’s pathophysiology involves intricate cellular changes in the pancreas, leading to uncontrolled cell growth and tumor formation. Genetic mutations and molecular alterations disrupt normal cellular regulation, promoting the survival and proliferation of cancer cells. The tumor microenvironment, comprising surrounding tissues and immune cells, further aids tumor progression by fostering angiogenesis and immune evasion. This hostile environment contributes to the disease’s aggressive behavior and resistance to treatment. Understanding the pathophysiological mechanisms at play is pivotal in developing targeted therapies that can interrupt the cancer’s growth signals, modulate the tumor microenvironment, and ultimately improve treatment outcomes for individuals affected by pancreatic cancer.
Types of Pancreatic Cancer
Pancreatic cancer encompasses diverse types, primarily pancreatic adenocarcinoma and neuroendocrine tumors (NETs). Pancreatic adenocarcinoma, the most common form, originates in the exocrine cells lining the pancreatic ducts and is notorious for its aggressive nature. In contrast, neuroendocrine tumors stem from hormone-producing cells within the pancreas and exhibit a slower growth rate. These tumors are further categorized as functional or non-functional based on hormone secretion. Less prevalent types include acinar cell carcinoma and adenosquamous carcinoma. The varying behavior, prognosis, and treatment responses of these pancreatic cancer subtypes emphasize the importance of accurate diagnosis and tailored management strategies to address the unique characteristics of each malignancy.
Clinical Presentation
Pancreatic cancer’s clinical presentation often evolves in a subtle and insidious manner. Early symptoms, such as unexplained weight loss, abdominal discomfort, and jaundice, may go unnoticed or be attributed to other conditions. As the disease advances, late-stage symptoms like severe pain, digestive difficulties, and back discomfort become prominent. These vague and non-specific signs pose diagnostic challenges, frequently leading to delayed detection. Recognizing the potential for pancreatic cancer in the presence of these symptoms is critical for early intervention. Improved awareness among healthcare professionals and the public is pivotal in ensuring timely diagnosis and treatment, ultimately enhancing the prognosis for individuals affected by this complex disease.
Diagnostic Approaches

Diagnostic approaches for pancreatic cancer involve a multi-pronged healthcare management strategy. Advanced imaging techniques, including CT scans, MRI, and endoscopic ultrasound, aid in visualizing tumors and determining their extent. Biopsies and pathological analyses provide definitive diagnoses. Tumor markers like CA 19–9 offer additional insights. Implementing these diagnostic tools in a coordinated healthcare management plan is crucial for accurate and timely identification of pancreatic cancer. Early detection can significantly impact treatment outcomes. Integrating these approaches into healthcare management protocols can enhance the efficiency of diagnosis, facilitate prompt initiation of treatment, and ultimately improve the prognosis for individuals facing the challenges of pancreatic cancer.
Staging and Prognosis
Staging and prognosis assessment are pivotal in guiding pancreatic cancer treatment strategies. Utilizing the TNM staging system, which considers tumor size, lymph node involvement, and metastasis, helps categorize the disease’s extent. Prognostic factors such as the stage at diagnosis, tumor resectability, and patient overall health influence treatment decisions and survival expectations. Unfortunately, most cases are diagnosed at advanced stages, limiting curative options. The five-year survival rates remain low due to aggressive tumor behavior and challenges posed by late-stage detection. However, advancements in treatment approaches, including surgery, chemotherapy, and targeted therapies, offer potential for improved outcomes. Combining accurate staging with individualized treatment plans offers the best chance at enhancing prognosis and quality of life for those affected by pancreatic cancer.
Treatment Options
Pancreatic cancer treatment options necessitate comprehensive hospital management strategies. Surgical interventions, like the Whipple procedure and distal pancreatectomy, aim to remove localized tumors. Chemotherapy regimens, such as gemcitabine and FOLFIRINOX, target cancer cells systemically. Radiation therapy is employed to shrink tumors before surgery or alleviate symptoms in advanced cases. Emerging targeted therapies and immunotherapies hold promise. Hospital management ensures coordinated care, addressing potential surgical complications, chemotherapy side effects, and radiation therapy planning. Palliative care offers supportive measures to enhance patients’ quality of life. Integrating these treatment modalities within hospital management protocols optimizes patient care and provides a multifaceted approach to tackle the challenges posed by pancreatic cancer.
Challenges in Treatment

Treatment of pancreatic cancer is marred by several challenges. Late-stage diagnosis is common due to vague symptoms, limiting curative options. Additionally, the cancer’s intrinsic resistance to chemotherapy and radiation often hampers treatment effectiveness. Surgical interventions can be complex and carry risks. Even successful surgeries may face complications like infections or post-operative pancreatic fistulas. The aggressive nature of the disease and its potential impact on patients’ overall health further complicate treatment decisions. Addressing these challenges requires a multidisciplinary approach, personalized treatment plans, and ongoing research efforts. Developing novel therapies, improving early detection methods, and enhancing supportive care can collectively mitigate the hurdles posed by pancreatic cancer treatment.
Research and Emerging Therapies
Continuing Werner Forssmann’s legacy, ongoing research harnesses advanced technologies to unlock innovative therapies. Cutting-edge studies explore genetic, cellular, and precision medicine approaches, reshaping healthcare. Emerging therapies, such as gene editing and personalized immunotherapies, show promise in treating previously untreatable diseases. These breakthroughs rely on interdisciplinary collaborations, integrating bioinformatics, nanotechnology, and advanced diagnostics. While challenges remain, the synergy of research and technology is paving the way for transformative changes in patient care. Inspired by Forssmann’s fearless curiosity, researchers continue to challenge conventions, forging new paths to address unmet medical needs and revolutionize the future of healthcare.
Prevention and Awareness
In the wake of Werner Forssmann’s legacy, emphasis on prevention and awareness is reshaping healthcare paradigms. Aided by modern technologies, proactive health monitoring and early intervention are gaining prominence. Public awareness campaigns educate communities about preventive measures, fostering healthier lifestyles and reducing disease burdens. Leveraging digital platforms and data analytics, healthcare systems can identify at-risk populations and tailor interventions. Forssmann’s audacious pursuit of medical advancement inspires a collective commitment to proactive healthcare practices. As prevention gains traction, his legacy serves as a reminder that empowering individuals with knowledge and promoting early detection are integral to shaping a healthier society and steering healthcare toward a future that prioritizes well-being.
Conclusion

In conclusion, Werner Forssmann’s pioneering spirit continues to reverberate through modern healthcare, inspiring innovation and patient-centric approaches. His legacy underscores the transformative potential of challenging norms and pushing scientific boundaries. Amid this legacy, QMe Healthcare Management and Information System stand as exemplars of this ethos, streamlining care delivery, enhancing patient experiences, and enabling personalized treatment strategies. As we look ahead, Forssmann’s journey reminds us that progress in healthcare stems from audacious curiosity and technological integration. By embracing his legacy and harnessing contemporary tools, we forge a path towards a healthcare future that honors tradition while embracing the transformative power of advanced systems for the betterment of patient well-being.
- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer