- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer
GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION.
GUARDING GUT HEALTH: YOUR GUIDE TO POTENTIAL CROHN’S DISEASE PREVENTION
INTRODUCTION
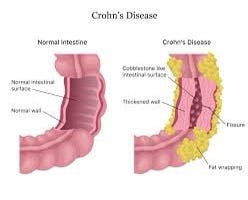
Crohn’s disease is a chronic inflammatory bowel disease (IBD) that primarily affects the digestive tract. It causes inflammation, irritation, and damage to the lining of the digestive tract, leading to a range of symptoms. Here’s some key information about Crohn’s disease: It should be noted that Crohn’s disease is a complex condition, and individual experiences can vary widely. If you suspect you have Crohn’s disease or have been diagnosed, it’s crucial to work closely with a healthcare provider to develop a personalized treatment plan that suits your needs.
CAUSES AND SYMPTOMS
CAUSES LEADING TO CROHN’S DISEASE
The exact cause of Crohn’s disease is not fully understood, but it is believed to involve a combination of genetic, immune system, and environmental factors:
1.Genetics: People with a family history of Crohn’s disease are at a higher risk. Certain genetic variations appear to increase susceptibility to the condition.
-
Immune System: Crohn’s disease is characterized by an abnormal immune response in which the immune system mistakenly attacks the healthy cells in the digestive tract. This leads to chronic inflammation.
-
Environmental Factors: Factors such as diet, smoking, and exposure to certain infections or pollutants might play a role in triggering or exacerbating the condition.
SPOTTING THE SYMPTOMS
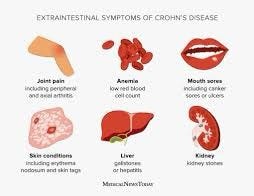
The symptoms of Crohn’s disease can vary widely from person to person and can also change over time. Common symptoms include:
1.Abdominal Pain: Persistent and often cramp-like abdominal pain is a hallmark symptom. It can range from mild discomfort to severe pain.
-
Diarrhea: Frequent, watery, or bloody stools are common. Diarrhea can be accompanied by urgency to use the bathroom.
-
Weight Loss: Chronic inflammation and reduced nutrient absorption can lead to unintended weight loss.
-
Fatigue: Inflammation and the body’s response to it can cause fatigue and a lack of energy.
-
Reduced Appetite: Loss of appetite and feeling full quickly after eating can occur due to inflammation affecting the digestive process.
-
Fever: Low-grade fever might be present during flare-ups as a result of inflammation.
-
Joint Pain: Joint pain, often resembling arthritis, can be a symptom, especially in the larger joints.
-
Skin Problems: Skin conditions like rashes, ulcers, and lesions might develop due to the inflammation.
-
Mouth Ulcers: Ulcers in the mouth can occur, resembling canker sores.
-
Perianal Complications: Inflammation around the anus can cause pain, swelling, and fistulas (abnormal connections between organs).
-
Delayed Growth in Children: In children, Crohn’s disease can lead to delayed growth and development.
It’s important to note that Crohn’s disease has a variable course, with periods of remission and flare-ups. Some individuals may experience only mild symptoms, while others may have more severe complications.
If you suspect you have Crohn’s disease or are experiencing any of these symptoms, it’s crucial to consult a gastroenterologist or healthcare provider for proper diagnosis and management. Crohn’s disease requires ongoing medical attention and treatment to help control inflammation, manage symptoms, and improve quality of life.
TREATMENT AND MEDICATIONS

Certainly, here’s a detailed overview of the treatment and medications commonly used for managing Crohn’s disease:
Treatment Approaches:
The treatment goals for Crohn’s disease are to control inflammation, manage symptoms, achieve remission (absence of symptoms), and improve quality of life. Treatment plans are tailored to each individual’s unique situation, considering factors such as the location and severity of inflammation, overall health, and response to previous treatments.
Medications:
Various medications are used to treat Crohn’s disease, depending on the severity and specific needs of the patient. Here are some of the medications commonly prescribed:
- Anti-Inflammatory Drugs:
Aminosalicylates: These drugs help reduce inflammation in the digestive tract. They are often used for mild to moderate cases and include mesalamine and sulfasalazine.
- Corticosteroids:
. – Prednisone, Budesonide: These medications are used to rapidly reduce inflammation and control symptoms during flare-ups. However, they are not typically used for long-term management due to potential side effects.
- Immunosuppressants:
. – Azathioprine, Mercaptopurine: These drugs suppress the immune system to reduce inflammation. They are used for maintaining remission and reducing the need for corticosteroids.
- Biologics (Monoclonal Antibodies):
. – Infliximab, Adalimumab, Vedolizumab, Ustekinumab: These medications target specific molecules involved in the immune response. They are effective for inducing and maintaining remission, especially in moderate to severe cases.
- Janus Kinase (JAK) Inhibitors:
. – Tofacitinib: A newer class of medications that suppress immune system activity and are used in certain cases of moderate to severe Crohn’s disease.
- Antibiotics:
. – Metronidazole, Ciprofloxacin: Antibiotics might be used to treat complications such as perianal fistulas or to address bacterial overgrowth.
- Pain Relievers and Antidiarrheals:
Acetaminophen, Loperamide: These medications might be used to manage pain or diarrhea, but NSAIDs (like ibuprofen) are generally avoided due to their potential to worsen symptoms.
Surgery:
In cases where medications don’t effectively control symptoms or complications arise, surgery might be necessary. Surgery can involve removing damaged portions of the digestive tract, repairing fistulas, or addressing blockages.
Lifestyle and Diet:
While medications play a significant role, lifestyle changes and dietary adjustments can also support Crohn’s disease management. Working with a dietitian to identify trigger foods, staying hydrated, and maintaining a balanced diet are important.
Remember that Crohn’s disease treatment is highly individualized. What works for one person might not be suitable for another. It’s crucial to work closely with a gastroenterologist or healthcare provider to develop a treatment plan tailored to your needs, monitor your progress, and make adjustments as necessary. Open communication with your healthcare team is key to managing this chronic condition effectively. Additionally, QMe offers packages support for various medical services and features automated billing to ensure transparent and hassle-free financial transactions. Embracing QMe empowers hospitals to enhance patient experiences, optimize healthcare workflows, and deliver top-notch medical services.
SURGERY AS A TREATMENT
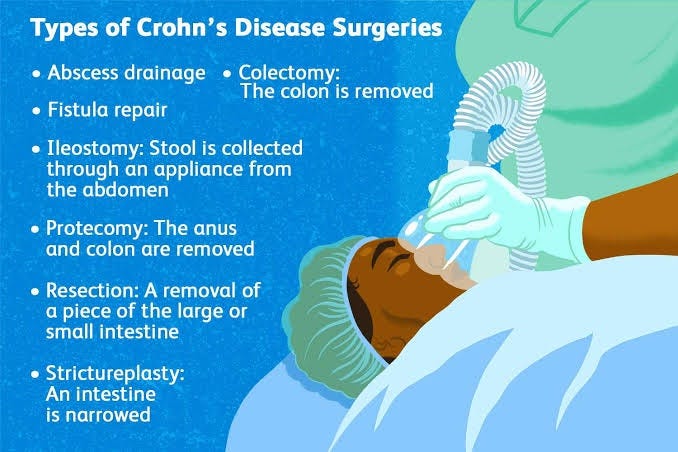
It is important to remember that surgery is a good treatment option for Crohn’s disease. It can help with improving quality of life and managing the disease. Surgery, however, is not a cure for Crohn’s disease.
Various Surgeries
Abscess drainage:
People with Crohn’s disease may be at a greater risk for abscesses. An abscess is when an infection causes a collection of pus. This might occur in the glands that surround the anus. Abscesses can be painful and difficult to cope with, so they might be drained to provide relief.
Colectomy:
During a colectomy, the colon is removed. Some or part of the rectum is left. If the colon is removed, stool will need to leave the body in another way. This procedure is done in one of two ways. One way is with an ileostomy, in which a piece of the small intestine is brought through an opening in the abdomen (called a stoma). The other way is called a straight pull-through. This is when the end of the small intestine is connected to the rectum.
Fistula repair:
A fistula is an abnormal connection between two organs. That can be, for instance, the colon and the skin or the colon and the vagina. Fistulas can happen for various reasons, but in Crohn’s disease, they usually involve the intestines.
There are different types of surgery used to treat fistulas. The procedure that’s used will depend on how extensive the fistula is and where it’s located. A colorectal surgeon will help in recommending which type of surgery might be done. A fistulotomy, for instance, might be done for a fistula in or around the anus that goes to the skin. A fistulectomy might be used when there’s a more complicated fistula between two organs.
Ileostomy:
An ileostomy is when a piece of the small intestine is brought through the abdomen and an appliance is worn over it to collect stool. It might be created after part or all of the large intestine is removed. An ileostomy can be temporary or permanent.
Proctectomy:
Proctectomy surgery is the removal of the anus and the rectum. The removal of these parts of the large intestine will mean that an ostomy is also created. A proctectomy might be done when Crohn’s disease affects the perianal area (the skin around the anus).3
Resection:
A resection is the removal of a piece of the small or the large intestine. The part that is inflamed or damaged is taken out. The two healthy ends of the intestine are then attached back together.
Strictureplasty:
A stricture is a narrowing in the intestine. This can occur because inflammation causes the wall of the intestine to thicken. It can also happen when the intestinal wall thickens because of scar tissue.
A narrowing can mean that a blockage is more likely. Opening up the stricture can be done surgically, and it doesn’t lead to a loss of any part of the bowel.
PREVENTATIVE MEASURES
Crohn’s disease is a complex condition, and while its exact cause isn’t fully understood, there are steps you can take to potentially reduce the risk or prevent its onset. Keep in mind that these measures aren’t guaranteed to prevent Crohn’s disease, but they may contribute to a healthier lifestyle:
-
Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help maintain gut health. Consider reducing processed foods, high sugar intake, and excessive fat.
-
Hydration: Staying hydrated supports overall digestive health. Drinking adequate water can help prevent inflammation and maintain proper bowel function.
-
Avoid Smoking: Smoking is a significant risk factor for Crohn’s disease. Quitting smoking can decrease your risk and also lead to better overall health.
-
Stress Management: Chronic stress doesn’t directly cause Crohn’s disease, but it can trigger flare-ups. Engaging in stress-relieving activities like exercise, meditation, yoga, or deep breathing can be beneficial.
-
Regular Exercise: Physical activity supports a healthy immune system and can help regulate digestion. Aim for regular exercise to maintain a healthy body.
-
Limit NSAIDs: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can worsen symptoms in people with Crohn’s disease. Limit their use if possible.
-
Antibiotic Use: Antibiotics might disrupt the balance of gut bacteria. Using antibiotics only when necessary and under medical supervision is advised.
-
Breastfeeding: If you’re a mother, breastfeeding your child might lower their risk of developing Crohn’s disease later in life.
-
Environmental Factors: Exposure to certain infections or environmental factors might contribute to Crohn’s disease. Maintaining good hygiene and avoiding contaminated water or food can help reduce exposure.
-
Regular Check-ups: If you have a family history of Crohn’s disease or other inflammatory bowel diseases, regular medical check-ups can help in early detection and management.
-
Genetic Counseling: If you have a family history of Crohn’s disease, consider genetic counseling to understand your risk better.
Remember, Crohn’s disease is influenced by a combination of genetic, environmental, and immunological factors. While these prevention tips might reduce the risk, they aren’t a guarantee. If you have concerns about Crohn’s disease, consult a healthcare professional for personalized advice.
CONCLUSION
In conclusion, while there is no foolproof method to prevent Crohn’s disease, adopting a healthy lifestyle can play a crucial role in reducing the risk of its onset and managing its symptoms. A well-balanced diet, proper hydration, stress management, regular exercise, and avoiding harmful habits like smoking are key components of a preventive approach. Genetic factors and environmental influences also play a role, so maintaining awareness and staying proactive with regular medical check-ups can aid in early detection and management. It’s important to remember that individual susceptibility varies, and consulting with healthcare professionals for personalized guidance is essential. It should be taken into consideration that QMe is a cutting-edge hospital management software designed to revolutionize healthcare facilities worldwide. With its intelligent queue-based OPD management system, patients experience reduced waiting times and optimized appointment scheduling. The software’s comprehensive patient history and electronic health records ensure seamless access to critical medical information, enabling healthcare professionals to make informed decisions and provide personalized care. QMe’s automatic workflows streamline administrative tasks and treatment plans, enhancing overall efficiency and reducing human errors. The software’s IPD management feature enables smooth inpatient care coordination, while its TPA support simplifies insurance processes.
- “Empowering Emergency Medicine Physicians”
- “Queue Management Software and Hospitalists in Modern Healthcare”
- “Enhancing-Pediatric-Infectious-Disease-Care”
- “Revolutionizing-Geriatric-Care”
- “Optimizing-Patient-Care-in-Pediatric-Rheumatology”
- “Pediatric-Pulmonology-Care”
- “Revolutionizing-Pediatric-Gastroenterology”
- “Enhancing-Pediatric-Neurology-Care”
- “Optimizing-Pediatric-Cardiology”
- “Enhancing-Pediatric-Endocrinology-Care”
- “Empowering-Neonatologists-with-EMR-Software”
- “Pediatrics-in-Focus”
- “Empowering-Neurologists-with-Electronic-Prescriptions”
- “Streamlining-Dermatology-Practice”
- “Streamlining-Psychiatry-Practice”
- “A-Game-Changer-for-Infectious-Disease-Specialists”
- “Allergist/Immunologist-Practices-with-QME-EMR-and-Hospital-Management-Systems”
- “Empowering-Hematologists-and-Revolutionizing-Healthcare-Management”
- “Optimizing-Healthcare-with-HMIS”
- “Transforming-Healthcare-with-Endocrinologist”
- “Healthcare-Management-with-QMe-EMR-for-Nephrologists”
- “Revolutionizing-Healthcare-Management-with-Cardiologist”
- “Streamlining-Operations-with-Queue-Management-Software”
- “Optimizing-Healthcare-Delivery”
- “Transforming-Healthcare-Management”
- HMIS And Decision Support Systems
- Dengue Unveiled: An Overview of Causes, Symptoms, and Prevention.
- Dengue Fever: Unraveling the Mosquito-Borne Menace.
- HMIS-and-Continuity-of-Care
- Project-Management-for-Successful-HMIS
- Catalysts of Wellness: The Transformative Power of Diagnosis and Screening in Healthcare
- Patient-Data-Management
- Guardians of Healthcare: The Vital Role of Fraud Detection in Ensuring Ethical Care
- Unlocking Insights
- Healthcare in the Digital Age: The History Of Development Of HMIS
- Transforming Healthcare
- Safeguarding-HMIS-Data
- HMIS-Integration-Challenges
- ANXIETY UNVEILED: CONQUERING FEARS AND CULTIVATING CALM.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- BEYOND THE BLUE: EMBRACING LIGHT ON THE PATH OF DEPRESSION.
- HMIS and Resource Allocation
- HMIS Data Accuracy and Integrity
- SOOTHING THE SILENT PAIN: UNDERSTANDING VULVODYNIA.
- Impact of HMIS on OPD Operations
- In Patient Management Through Health Management
- WITHIN THE SHADOWS: UNDERSTANDING BRAIN TUMOURS FROM WITHIN
- HMIS-and-Health-Insurance-Integration
- HMIS-Data-Analytics-for-Preventive-Care
- SILENT INTRUDERS: UNRAVELLING THE MYSTERIES OF PELVIC INFLAMMATORY DISEASE
- BREAKING FREE: OVERCOMING THE HURDLE OF URINARY INCONTINENCE
- “HMIS and Doctor-Patient Communication”
- HEALING INSIGHTS: THE POWER OF THE HOSPITAL MANAGEMENT INFORMATION SYSTEM.
- SOLVING THE OVARIAN PUZZLE:UNDERSTANDING OVARIAN CYST INSIDE OUT
- Usability And User Experience In HMIS
- WARRIOR’S BATTLE: TRIUMPHING OVER UTERINE CANCER
- POLYCYSTIC OVARY PUZZLE: UNRAVELLING THE ENIGMA OF PCOS
- Unlocking-the-Potential-of-HMIS-Data-for Medical-Research-and-Healthcare-Policy-Enhancement
- Feminine Health Unplugged: Empowering Women in Vaginal Infection Awareness
- Revitalizing Feminine Comfort: A Journey Through Vaginal Wellness.
- HMIS Vendor Selection Guide
- UNDERSTANDING FIBROIDS: NAVIGATING THE INTRICACIES OF UTERINE HEALTH.
- Best Practices for Data Migration in Healthcare Management Information Systems (HMIS)
- CONCEIVING HOPE: NAVIGATING THE JOURNEY OF INFERTILITY
- MENSTRUAL IRREGULARITIES: CAUSES AND TREATMENT
- RISING ABOVE: EMPOWERING WOMEN WITH PELVIC ORGAN PROLAPSE
- Leveraging HMIS for Enhanced Public Health Management and Disease Surveillance
- Challenges and Benefits of Implementing HMIS in Rural and Remote Healthcare Settings
- Securing Healthcare Continuity
- Pancreatic Cancer
- Lymphoma
- Leukemia
- Bladder Cancer
- Skin Cancer (Melanoma)
- COLORECTAL CANCER
- All about Prostate Cancer
- Fighting out the Disease of Lung Cancer
- Advances in Breast Cancer Treatment: A Comprehensive Guide
- Autism Spectrum Disorder (ASD)
- EHR SYMPHONY: HARMONIZING HEALTHCARE THROUGH ELECTRONIC RECORDS .
- Understanding Testicular Cancer: Detection, Treatment And Awareness.
- Childhood Obesity
- Kawasaki Disease
- Eczema (Atopic Dermatitis)
- Understanding Bone Cancer: A Brief Overview.
- Virtual Healing: Navigating Healthcare Through Telemedicine and Telehealth.
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- PELVIC PAIN:CAUSES SYMPTOMS AND PREVENTIONS
- Type 1 Diabetes: Causes, Symptoms, and Treatment
- Gastroesophageal Reflux Disease (GERD)
- Battling Pneumonia: Unveiling the Stealthy Invader of the Lungs
- Unravelling the Complexity of Allergic Reactions: Understanding, Managing, and Thriving
- Rashes (Eczema, Dermatitis)
- UNDERSTANDING CERVICAL DYSPLASIA: CAUSES, SYMPTOMS AND MANAGEMENT
- Chicken Pox
- Endometriosis Unmasked: A Closer Look at the Silent Struggle
- Croup
- Hand, Foot and Mouth Disease (HFMD)
- THE DAWNING OF A NEW ERA: EMBRACING THE JOURNEY OF MENOPAUSE
- Urinary Tract Infections (UTIs)
- Strep Throat (Streptococcal Pharyngitis)
- Understanding Otitis Media(Ear Infection)
- 28th July In medical history!!
- Influenza (Flu) - Symptoms, Prevention and Management
- 27th July In medical history!!
- Respiratory Syncytial Virus (RSV) Infection
- SIGNIFICANCE AND ADVANTAGES OF HMIS: A DETAILED ANALYSIS
- Beyond Boundaries: Transforming Healthcare with Virtual Reality
- TRACK YOUR LIFE : A DETAILED UNDERSTANDING ON HEALTH MONITORING SYSTEM
- EXPLORING BENEATH THE SURFACE: UNDERSTANDING BARTHOLIN CYSTS AND ABSCESSES
- PATHWAYS OF HOPE: NAVIGATING THE CHALLENGES OF ESOPHAGEAL CANCER
- Gastric Battles: Confronting Stomach Cancer Head-On.
- HMIS IN SMALL CLINICS: A STEP TO A BETTER FUTURE
- Harmonizing Your Cycle: A Journey to Menstrual Health and Balance.
- Respiratory Syncytial Virus (RSV) Infection
- GUARDING OUR INTIMATE WORLD: A CLOSER LOOK AT STI
- Real-World HMIS Implementation Case Studies: Using Data to Transform Healthcare
- Gastroenteritis (Stomach Flu)
- Asthama - The Anatomy Of Breathing
- Influenza - A Silent Intruder
- Breast Cancer